A Case Study on PCOS
GLOBAL JOURNAL OF REPRODUCTIVE
MEDICINE-JUNIPER PUBLISHERS
Abstract
Polycystic ovary syndrome (PCOS)is a condition in which the ovaries produce an abnormal amount of androgens, male sex hormones that are usually present in women in small amounts. Features of PCOS in this case are oligomenorrhoea and left ovary bulky (not meeting criteria of Rottadarm,10cm size, >10 follicles, >10 mm follicles). Her symptoms aggravated leading to hospitalization with hypoglycaemia. Initial work up showed decreased gonadtrotpins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia. Initial work up showed decreased gonadtrotpins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia and has normalization of FSH, LH, Estradiol and prolactin with normal insulin levels. Clinical and biochemical profile is suggestive of functional Hypothalamic Amenorrhoea.
Introduction
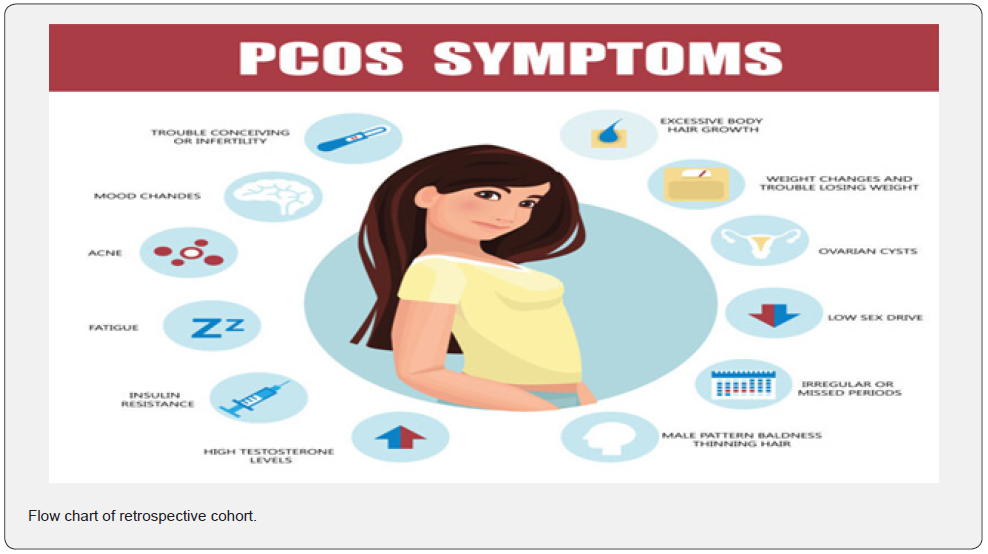
PCOS is extremely prevalent and probably constitutes the most frequently encountered endocrine (hormone)disorder in women of reproductive age. Having the disorder may significantly impact the quality of life of women during the reproductive years, and it contributes to morbidity and mortality by the time of menopause. PCOS women are at increased risk for CHD and T2 DM. PCOS women should undergo screening for HTN, abnormal lipid profiles, insulin resistance, and reproductive disorders including cancer of endometrium. PCOS symptoms were first described and documented by the Italian physician Antonio Vallisneri in 1721 (Figure 2).
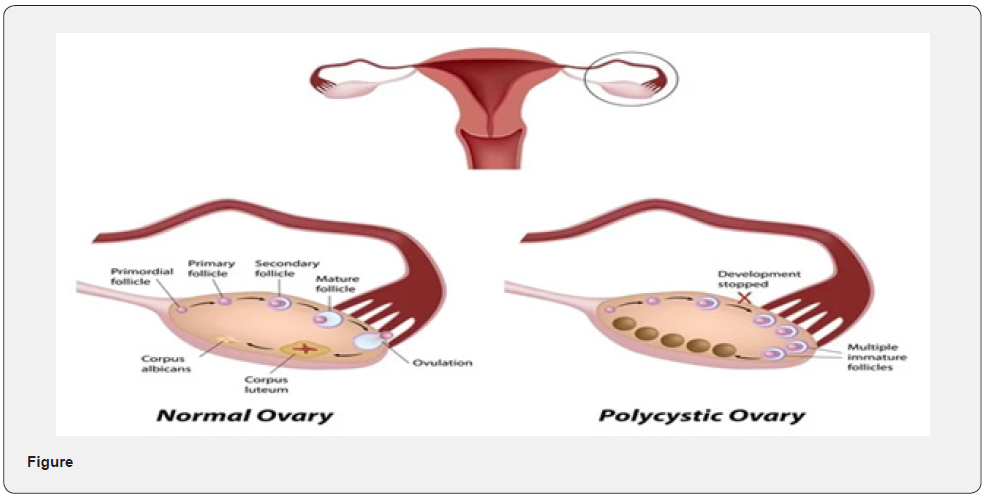
What is PCOS?
A hormonal disorder causing enlarged ovaries with small cysts on the outer edges. Polycystic ovary syndrome (PCOS)is a condition in which the ovaries produce an abnormal amount of androgens, male sex hormones that are usually present in women in small amounts. The name PCOS describes the numerous small cysts (fluid-filled sacs) that form in the ovaries.
Goal
• Help patient to perceived change in body structure.
Intervention:
• Assess the perceived impact of change in body
• Provide psychological support.
• Help identify actual changes and discuss the changes whether its permanent or temporary.
Imbalanced nutrition more than body requirement related to intake of OCP’s as evidenced by weight gain and increase BMI.
Goal
• To reduce weight.
Intervention
• Assess patients BMI
• Assess eating pattern
• Review daily activity and exercise
• Encourage patient to chose nutritious food such as green vegetables, fruits and low fat food.
Anxiety related to disease process as evidenced by frequently asking question.
Goal
• To reduce anxiety
Intervention
• Assess the level of anxiety.
• Provide psychological support
• Explain about the disease process
• Establish basis for comfort in communicating anxious feeling
• Encourage involvement in planned exercise programmed
• Provide information regarding poor dietary habits
A Case Study
20 yr old client Ms. mon, hospitalized in base hospital with three episode of hypoglycemia in last 24 hours.On early morning hours at 0200hrs (28 sep 2022)in the hostel. she felt sweating, tremors of hand and dizziness for which she felt better after taking chocolates and biscuit and following that day during duty hours, she felt dizziness with sweating and RBS-69mg/dl. she was managed with i.v dextrose saline and oral glucose after which she felt better and was sent home with an advice to get OGTT next day. On 29 sep 2022 at 1115 hrs when she was giving blood after OGTT (75mg glucose). she felt dizziness with sweating and RBS was 32mg/dl by glucometer (venous blood sample at same time after 75 OGTT was 36mg/dl).Her symptoms improved with dextrose infusion and repeat BS was 177mg/l. She denied any intake of antidiabetic medications or any other supplements except for 21 days OCP which ended on 17Sep 2022. She felt similar episode of dizziness on 25 Aug 2022.She gave history that she noticed in the past 02 yr that a day before the cycle she feels very weak with sweating and self observation that the following day her cycle occur, though they have been irregular with 30-50 days gap. These symptoms were also present when menstrual cycle were assumed on OCP.
During hospital stay with continuous glucose monitoring sensor blood sugar levels ranged between 60-100mg/dl associated with sensation of weakness, hunger when blood sugar is below 70mg/dl.
She was allowed to take meals 02 hourly and spontaneous episode of hypoglycaemia occurred <60 mg/dl, blood sample was collected at 0100 am when blood sugar was 58 mg/dl by capillary method). Report was available on the next day and showed Cpeptide2.65mg/ dl (NO.1-5.19), corresponding S. Insulin was high 77.0MI/I (N:2-25) suggestive on endogenous hyperinsulinaemia. She was continued on small frequent meals. She also gave history of taking OCP, 21day cycle for PCOS from gynaecologist since Oct 2021when her menstrual cycle got delayed for more than 02months (USG pelvis left ovary bulky with small peripheral follicles, Rt ovary not fully visualized –MRI random pelvis done later showed both ovaries enlarged with peripherally placed follicles left>right). Attained menarche at 11yr of age onwards there was delay in her periods. Earlier work up in civil was told to have polycystic ovaries and had been advised exercise. She has no phenotypic features of PCOS and no clinical hyperandrogenism. She took homeopathic medication for one month, jul-aug and stopped. She also gave history of being under stress due to academics and being away from home. she had an episode of anxiety last year for which she was admitted and evaluated with no organic cause found. she was counselled by psychological counsellor. There was no recurrence of anxiety symptoms. However, she gave history falling ill frequently in the form of not feeling like eating, nauseating sensation for a week and used to settle down on its own which coincided with delay in menstrual periods and menstrual periods resumed with intake of OCP’S.
The other hormonal analysis showed normal thyroid profile, decreased FSH, decreased LH, decreased Estrogen and raised prolactin levels. In the setting of hypoglycaemia with decreased pituitary hormones possibility of MEN-1 kept with other diagnosis of functional hypothalamic Amenrrohoea after all known causes excluded. MRI pituitary and sella showed normal sized pituitary for her age, no features suggestive of hypophysisits. She underwent behavioural counselling in view of decreased energy intake due to stress effects likely leading to hypoglycaemia. After 3rd day of admission there were no episodes of spontaneous hypoglycaemia.
She attained menstrual cycle after one day of admission lasting for a day. Repeat hormonal testing is done on D7 of menstrual cycle and extended OGTT. During extended OGTT the capillary blood sugar reading is 60mg/dl, blood samples are collected for venous blood sugar, C-peptide and low serum Insulin levels which showed 53 mg/dl hypoglycaemia, low normal c-peptide and low normal serum insulin levels suggestive of appropriate physiological response for hypoglycaemia and no biochemical evidence of endogenous hypoglycaemia. Repeat thyroid profile FSH, LH, S. estrogen, S. prolactin levels are normal. S. testosterone levels, Anti mullerian hormone values are normal. She has been advised to have regular meals and advised not to skip.
Presently she has no complaints of headache, palpitation, diaphoresis or increased hunger. She requires OPD follow up for any recurrence of symptoms and menstrual irregularities.
Clinical Findings
Thin body built, weight: 74kg, height -154 cm, BMI:19.8kg/m2, BP-127/76mmHg, no pallor/cyanosis/icterus/lymphadenopathy. No acanthosis nigricans, No goitre, No delayed tendon reflex. No cutaneous markers of turners syndrome. Chest –clinically clear :CVS:S1,S2 heard normal, abdomen – no organomegaly.
Investigations
Hb-11.6
TLC/ccmm-8000
P%L%-53,40
Plt/cumm-412000
Urea /S.creatinine -10/0.6mg/dl
Na/K meq/dl-143/4.6
S.bi/AST/ALT-0.5/10/15
S.chol/TG/LDL/HDL mg/dl-121/63/60/50
HbA1c-5.4%
MRI: Pituitary appears normal in size and signal characteristics and shows minimally convex outlines with maximum cranio– caudal dimension of 7.1 mm. Linfundibular stalk 3.3 mm at the level of optic chiasm and 1.9 mm just above the gland.
USG Pelvis: Uterus normal in size and echotexture. The endometrial thickness measures 5.5mm. Left ovary measures 8.3cc in volume with few peripherally located follicles and increased stromal echogenicity. Right ovary is not well visualized. Bilateral adnexa appear normal. Radiologist opined as polycystic appearance of left ovary. USG abdomen showed liver size -16.2 cm in CC axis, hepatomegaly ECG, urine RE, CXR-PA view: Normal.Discussion
Young girl history of academic stress and occurrence of irregular cycle, episodes of vomiting sensation, decreased food intake for about a week. These episodes used to occur every month. She has no phenotypic features of PCOS except for oligomenorrhoea and left ovary bulky (not meeting criteria of Rottadarm,10cm size, >10 follicles, >10 mm follicles). Her symptoms aggravated leading to hospitalization with hypoglycaemia. Initial work up showed decreased gonadotropins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia. Initial work up showed decreased gonadotropins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia and has normalization of FSH, LH, Estradiol and prolactin with normal insulin levels. Clinical and biochemical profile is suggestive of functional Hypothalamic Amenorrhoea [1-4].
Treatment Advised
1. Small frequent complex carbohydrate meals as advised in diet chart
2. Watch for any episodes of hypoglycaemia
3. Follow up by endocrinologist for further follow up
4. Can be considered for behavioural therapy
Conclusion
PCOS is extremely prevalent and probably constitutes the most frequently encountered endocrine (hormone) disorder in women of reproductive age. PCOS is one of the most common causes of female infertility, affecting 6% to 12% (as many as 5 million) of US women of reproductive age. It affects 4% - 20% of women of reproductive age worldwide.
Read
More About This Article: https://juniperpublishers.com/gjorm/GJORM.MS.ID.555761.php
To know more about Global
Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php


Comments
Post a Comment