Homocysteine as a Predictor of Preeclampsia
GLOBAL JOURNAL OF REPRODUCTIVE
MEDICINE-JUNIPER PUBLISHERS
Abstract
Homocysteine is an amino acid that is a product of methionine metabolism, is related to preeclampsia in 20-30%, the increase of this or hyperhomocysteinemia may result from the genetic defect of the enzyme methylenetetrahydrofolate reductase involved in the synthesis of homocysteine. Maternal mortality due to preeclampsia is up to 44% and perinatal mortality is reported at up to 27.8%. The objective of this research was to determine homocysteine levels as a predictor of preeclampsia in pregnant women 12 to 20 weeks pregnant. This was an observational, longitudinal and prospective investigation. The study population were patients attending the first antenatal care consultation between 12 to 20ava. weeks, the sample was random that included 360 patients who determined serum homocysteine Sand excluded 48 patients whodid not meet the inclusion and exclusion criteria; they found homogeneity among the patients, 270 patients (86.5%) had a normal evolutionary pregnancy, 27 patients (8.65%) had gestational hypertension, 9 (2.88%) mild preeclampsia and 6 patients (1.9%) severe preeclampsia, none developed HELLP syndrome. Increased homocysteine levels were found in 9 patients who were not related to hypertensive pregnancy disorders. In the present research, homocysteine was not shown to be a predictor of hypertensive disease in pregnancy.
Introduction
Preeclampsia (PE) - eclampsia is a hypertensive disorder of placental origin of unknown cause. Various theories have been considered because none, by itself, explains the variety of pathophysiological events that characterize it. The hereditary, acquired, familial, environmental, immunological, and individual factors attributed to it appear to interact in various ways to make it appear. It is also suggested that the common denominator in it is utero-placental ischemia from an incomplete replacement of the muscular layer of the wall of the spiral arterioles (terminal branches of the uterine arteries) by trophoblastic cells at 12 weeks at 14 and 16 to 18 of gestation [1].
It has been found that alterations in methionine- homocysteine (Hci) metabolism may be related to systematic vascular damage, which can lead to the classic clinical appearance of hypertensive disorders of pregnancy. It is also assumed that high levels of Hci can contribute to the development of placental microvascular diseases and PE, negatively affecting the endothelium. Women diagnosed with PE are at higher risk of future cardiovascular or cerebrovascular disease, compared to unaffected women.
Hyperhomocysteinemia acts as a risk factor for cardiovascular disease; peripheral vascular; cerebrovascular disease, cognitive-dementia disorders; neurodegenerative and fractures associated with osteoporosis and could have a genetic origin or related to folate deficiency [2]. The cause of hyperhomocysteinemia in preeclampsia has been attributed to a decrease in folate concentration, secondary to a deficient intake of folic acid or an alteration in the metabolism of the enzyme methylene tehydrofolate ductase (MTHFR). Other possible mechanisms may be underlying metabolic syndrome, tissue damage, oxidative stress, and inflammation. Only a few authors consider that this increase is due to the increase in xanthine oxidase activity [2].
HCI is the method used to measure the serum of a pregnant women with a reference value of up to 10 mmol / dl. The association of homocysteine with vascular disorders is an issue that has been causing an impact in the last decades; A study carried out determined that11 of 58 severe PEs (19%) before 28 weeks of gestation had high homocysteine levels. Plasma homocysteine concentrations are significantly elevated in pregnant women with preeclampsia compared to healthy pregnant women during the third trimester of gestation. The prevalence of hyperhomocysteinemia is significantly higher in patients with preeclampsia compared to the control group [3]. Hyperhomocysteinemia is a risk factor for the development of PE due to the increased sensitivity of the uterus-placental vasculature during pregnancy; this can persist after pregnancy and predispose to late vascular disease or coronary artery disease at any stage of life. Some predictive risk factors have been described for the development of PE before its clinical presentation [4].
According to these antecedents, it has been observed that there are risk factors that are related to this pathology of pregnancy, which has a high rate of maternal perinatal mortality (MMP), but the etiological situation and the way to predict it is not yet clear. Some algorithms have been developed to predict PE, they are encouraging and must be validated. Simple preventive measures, such as low-dose aspirin, calcium, and diet and lifestyle interventions, show some potential benefit [5].
According to the World Bank (2014), the average expenditure on health care is estimated to be $ 579 per year per person in lowincome countries; and the protocols of preconception care are not carried out and if they exist they are deficient, thus we observe that the preconception and postconception folic acid supplementation do not follow the international protocols; in pregnancy pathologies, screening is not performed in asymptomatic stages such as gestational diabetes and DHE [6]. In our country and particularly in the University Hospital of Guayaquil (HUG) there are no preconception care programs, likewise prenatal care is deficient and routine control programs are not adequate in patients with regard to folic acid dosage and the determination of Hci in serum; the patients usually go to the first prenatal control from the second trimester.
Hyperhomocysteinemia is one of the signs associated with preeclampsia, but considering it as a predictive tool is a matter of debate. The objective of this research was to analyze the relationship between hyperhomocysteinemia in the first trimester of pregnancy and pre-eclampsia to consider it as a predictive method during pregnancy.
Material and Methods
Descriptive, observational, prospective, longitudinal-cut study in patients who attended the obstetric outpatient clinic of the Hospital Universitario de Guayaquil Ecuador from October 2018 - October 2019.
The analyzed universe consisted of 360 pregnant women between 12 and 20 weeks of gestation. A peripheral blood sample was taken with prior informed consent to quantify serum homocysteine levels and correlate whether high levels were related to the development of pre-eclampsia or another hypertensive disorder of pregnancy, the selected sample was of 312 patients who met the criteria of inclusion and exclusion Patients treated at the same hospital institution who had other associated diseases during pregnancy, those who did not have adequate follow-up by medical history, and those who ended their pregnancy at another institution were excluded.
Hyperhomocysteinemia was selected as the independent variable and hypertensive disorders of pregnancy were selected as the dependent variable. Among the unrelated variables were: body mass index (BMI), birth weight and maternal morbidity. Descriptive means were determined for quantitative variables: arithmetic mean and standard deviation. The qualitative variables were determined the absolute frequency and percentage. To establish an association between qualitative variables, the Chi square was determined. In all cases we worked for a significance level α = 0.05. The variables under study were processed in an SPSS statistical package.
Techniques and Procedures
Peripheral blood samples were taken from the patients in the 12 to 20 weeks of gestation in the clinical laboratory of the hospital in order to determine the serum levels of homocysteine; for which homocysteine levels of 12 umol / dL were taken as a cohort point. Preeclampsia was considered to be any patient who presented blood pressure figures of 140/90 mm Hg or more, verified at least twice in a period of 4-6 hours, after 20 weeks of pregnancy with proteinuria: ≥300 mg in 24 hours.
Ethical Procedures
The consent of the Scientific Council of the Unit where the research was carried out, the Research Ethics Committee and the Technical Council of the Hospital were taken into account, in addition to the provisions of the Helsinki agreements and the Medical Ethics regulations.
Results
Of the total of 360 women who attended the HUG obstetrics consultation for prenatal control in the first trimester of pregnancy, 48 patients who did not meet the inclusion criteria were excluded, because they had a history of hypertension, cardiovascular disease, diabetes mellitus, current multiple pregnancy, anti-folate drug treatment, diagnosed kidney disease and over 40 years of age, leaving 312 patients for the study. See Tables 1 & 2. 58% of the patients were from urban areas, 23% from rural areas; 19% of the marginal urban area.
72 patients had more than two previous partners, which corresponds to 23.1%; systolic blood pressure, as well as diastolic blood pressure, did not show significant alterations. The study population had the same characteristics in the intake of folic acid. With respect to the risk factors studied, we observe maternal age, parity, the low intake of foods rich in folates has an important value. See Table 2, Homocysteine values were taken in referenceto- reference values (5-13um / L). The most important variable of interest, identified as the proportion of DHE, did not become statistically significant (P 0.454), observing a 13.5% prevalence of hypertensive disease (Tables 3 & 4).
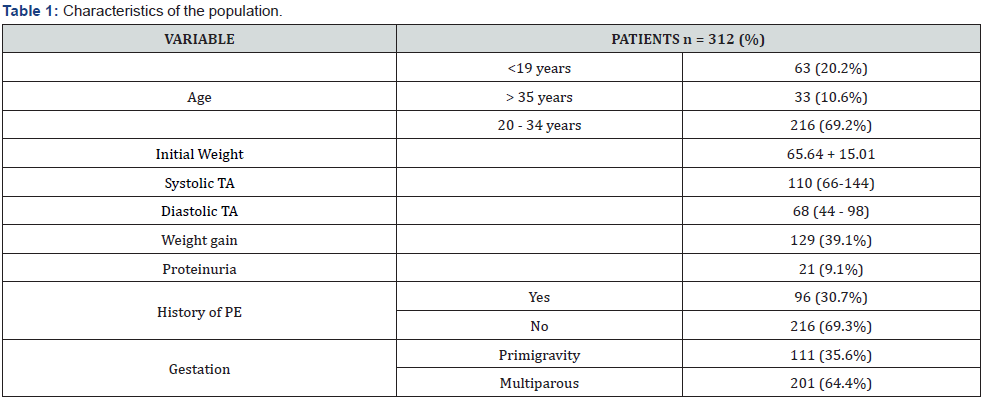
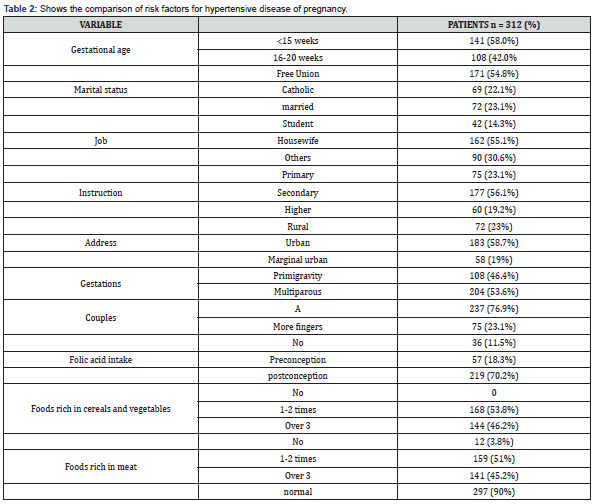
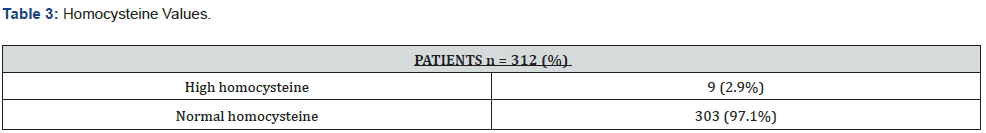
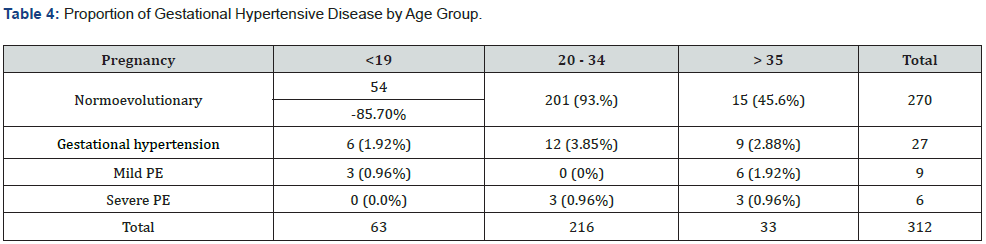
Table 1 describes the initial values of the study in terms of age, weight, blood pressure, history of PE and number of pregnancies. Table 2 shows the comparison of risk factors for hypertensive disease of pregnancy.
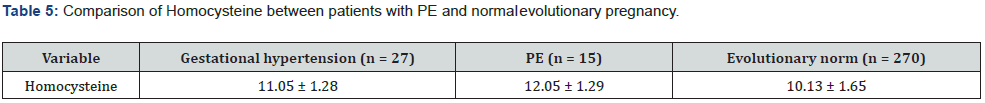
Of the 312 pregnant women, 270 (86.5%) had a normalevolutionary pregnancy, 27 patients (8.7%) had gestational hypertension, 9 (2.9%) had mild PE and 6 patients (1.9%) had severe PE, proteinuria 21 (6, 7%) none developed HELLP syndrome. Homocysteine values did not show significant values, of the 312 pregnant women only 9 patients (2.7%) had elevated serum homocysteine that ranged from 13 to 15 μmol / L, and 303 patients (84.5%) had homocysteine values of 5 to 12 μmol. Of the 312 patients who participated in the study, it reveals that 15 of them (4.8%) developed PE. These patients and those who presented a normal evolutionary pregnancy show Hci levels without statistical differences (p 0.0088) in patients with PE. and (p 0.03766518) in patients with gestational hypertension (Table 5).
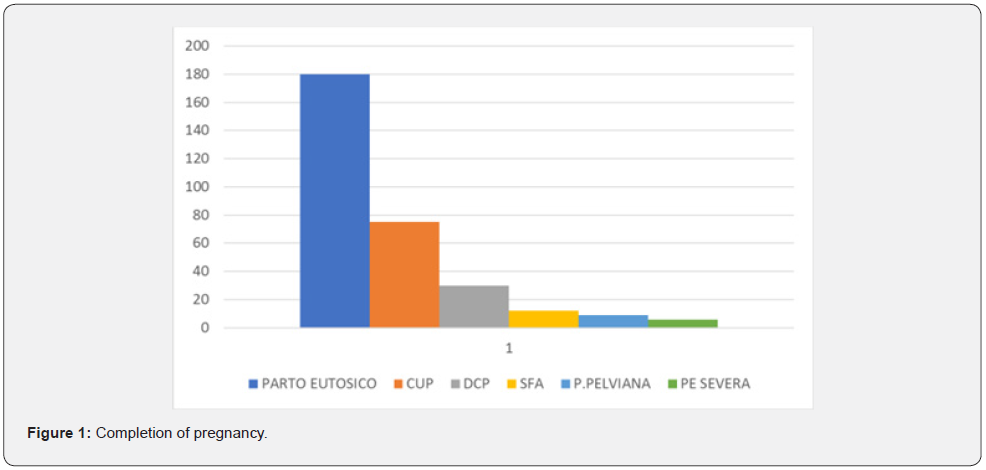
These results give us a sensitivity of 28.12% and a specificity of 47.12% as well as a positive predictive value of 2.29% and a negative predictive value of 49.52% for PE. The culmination of pregnancy was uncomplicated in all patients, they continued with periodic prenatal controls, as well as the intake of iron, calcium and folic acid. Regarding the type of delivery triggered in our sample, the following results were obtained: 57.7% of the pregnant women ended in eutocic delivery and 42.3% in caesarean section. The main indications for cesarean section were: 22.7% for presenting cephalopelvic disproportion due to pelvic narrowing, 56.8% for having had a previous cesarean section, 9.1% for acute fetal distress, 6.8% for pelvic presentation, and 4.5% as a consequence of severe PE. See graph 1. The mean weight of the newborns was 3227 ± 407 g Figure 1.
Discussion
DHE stand out as the main causes of MMP, the relationship with risk factors is well known and it is verified in the literature that the extremes of the reproductive life of women are associated with DHE [7,8], however, our study did not identify women under 19 or over 35 as risk factors. For decades of research on the disease and the ability of clinicians to predict PE, prior to the onset of symptoms, it has not significantly improved [9-11]. Guven et al in 2009, demonstrated that Hci levels are higher in patients with pre-eclampsia in the third trimester compared to those of healthy pregnant women [12], therefore it has been suggested that Hci levels could be used as predictors of pre-eclampsia [3,13-19].
Other studies also describe high levels of Hci in early pregnancies, associating them with the later development of mild PE [7], Kharb et al. Found that levels of Hci were slightly higher in the maternal blood of hypertensive pregnant women compared to the Normotensive pregnant women (p <0.001, p> 0.05 respectively). Mujawar et al. showed that serum Hci, folic acid and vitamin B12 levels are altered in pre-eclampsia [20-24], and the situation of hyperhomocysteinemia together with low levels of folic acid is related to PE [6,25]. But the study published with Wadhwani et al. which assesses the levels of maternal plasma folate, vitamin B 12 and Hci in women with normotensive control (NC) and women with PE from early pregnancy to delivery [26]. Maternal plasma homocysteine levels were higher in PE compared to NC at all time points These results indicate that there are higher levels of homocysteine in women with PE from early pregnancy and continue until delivery, these results being discordant with those of the present research work. Andrey et al. revealed that Hci levels are altered in uncomplicated and complicated pregnancy, in some reviews they tend to decrease in the second and third trimesters of pregnancy [27]. these results being discordant with those of the present research work. Andrey et al. revealed that Hci levels are altered in uncomplicated and complicated pregnancy, in some reviews they tend to decrease in the second and third trimesters of pregnancy [27]. these results being discordant with those of the present research work. Andrey et al. revealed that Hci levels are altered in uncomplicated and complicated pregnancy, in some reviews they tend to decrease in the second and third trimesters of pregnancy [27].
The present investigation did not find an increase in homocysteine, hyperhomocysteinemia was increased in 9 patients studied who did not develop PE. Sun F et al. revealed that hyperhomocysteine concentration in the first trimester is an independent risk factor for severe PE [28]. These results gave us a sensitivity of 28.12% and a specificity of 47.12% as well as a positive predictive value of 2.29% and a negative predictive value of 49.52% for PE.
Vitamin B12 levels were lower in the maternal blood of hypertensive pregnant women compared to normotensive pregnant women, concluding that folate and vitamin B12 deficiency and elevated Hci during pregnancy may be a risk factor for PE and a future cardiovascular risk [29]. However, our findings do not agree with these publications, since Hci levels did not establish a direct relationship with the development of PE, which would be explained by a diet enriched with folic acid, as well as the supplementation of 5 mg of folic acid from entered the study, the patients made their presentation decrease. In this sense, the recommendation to administer folic acid supplements to reduce the possibility of PE, and lower homocysteinemia concentrations, has not been successful in our work, therefore, we can compare our results to those published by Mujawar et al. in 2011 [24].
In the USA, 20% do not consume folic acid supplements and its incidence is the same as that of the rest of the population, which supports the observation that folic acid levels do not have a predictive role for the development of PE [12]. Today it is accepted that hyperhomocysteinemia is a cardiovascular risk factor, causing endothelial damage through veins and arteries due to a decreased capacity to incorporate deoxyuridine, including the placental vasculature, for this reason it is important to consider higher dosages of folic acid during pregnancy, as a protective factor for the appearance of pre-eclampsia [20,30]. Supplementation of folic acid with L- arginine could prevent PE by improving endothelial function [1].
It can be seen the evidence of hyperhomocysteinemia as a predictor of PE in pregnant women. Our study did not provide significant results since their foods are fortified with folic acid; this suggests that exogenous folic acid administration does not have a significant impact on the development of PE. This allows us to guide randomized, blinded and placebo studies to really establish the dose and its relationship with PE. Currently, the recommended daily dose of folic acid to reduce the risks of neural tube closure defects is 1 to 5mg daily [31].
As we know, DHE are one of the main causes of MMP, with significant chronic disability and death in mothers, as well as important and serious complications in the newborn that include prematurity, delayed intrauterine growth, and placental abruption. So far there are no preventive or curative strategies for these conditions [1,2,7,32,33]. The need to reduce the incidence of maternal and fetal complications from DUS is a health priority.
It is estimated that only in Ecuador in 2013 there were 43 deaths from this cause, with an estimated maternal mortality rate of 43 for every 340,000 live births [34]. On the other hand, the incidence of PE in its two varieties, mild or severe, is from 5 to 8%, or even up to 10%, with a significant rate of maternal and fetal mortality, as well as prematurity, delay in intrauterine growth and placental abruption [35,36].
The incidence of DUS found in the present work was 13.5%, similar to that reported in the literature, a percentage of which 8.7% corresponds to gestational hypertension, 4.8% to PE. As with the sociodemographic, personal pathological and gynecologicalobstetric risk factors, no significant differences were found (p 0.0088) and neither with what was published in the literature [33].
The study presented several limitations, in the beginning we proposed to achieve a larger sample size. In addition, it was shown that high doses of folic acid did not reduce the PE index, and a trend towards the opposite was observed, with higher proportions of hypertensive disease in pregnancy, although not statistically significant. We believe that this result is caused by the first limitation raised, for which a study is proposed in search of equivalences regarding hypertensive diseases of pregnancy.
Conclusion
Finally, we can say that hypertensive disorders of pregnancy are a public health problem, particularly PE and eclampsia, as they are considered the second cause of maternal death in the world. We have observed the effectiveness of hyperhomocysteinemia through specificity, sensitivity, positive and negative predictive value as a predictor of preeclampsia, taking into consideration the sensitivity of 28.12% and the specificity of 47.12%, the positive predictive value for PE was 2.29% and predictive value negative of 49.52%, for which we consider that the test is not specific or sensitive to predict preeclampsia in the present investigation.
Recommendation
Homocysteine can be used in first-level health, which in conjunction with other risk factors can improve the suspicion of the development of hypertensive disorders of pregnancy and therefore avoid complications with timely prophylactic treatment. It is necessary to carry out other experimental studies in which pregnant women at risk of suffering from preeclampsia and hyperhomocysteine are identified and treated prophylactically with low-salt diets, changes in lifestyles and breaks in the left lateral decubitus position, in this way the effectiveness of homocysteine to reduce the prevalence of this disease could be better evidenced. The use of homocysteine with a larger population in multicenter studies is recommended in order to increase the sample size and decrease the degree of imprecision and variability shown in the present study.
To know more about Global
Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php


Comments
Post a Comment