Molar Twin Deliveries with Coexisting Fetus at Term: Concerning Two Uncomplicated Cases of Gestational Trophoblastic Tumor, From 2015-2021, In Conakry, Guinea
GLOBAL JOURNAL OF REPRODUCTIVE
MEDICINE-JUNIPER PUBLISHERS
Abstract
The coexistence of a molar pregnancy with a live fetus is a rare entity of difficult diagnosis and treatment. Continuation of the pregnancy until full-term delivery is possible. We report two cases of twin molar deliveries observed empirically from 2015-2021, in the gynecology-obstetrics department of the Donka national hospital and in the maternity ward of the Jean Paul II hospital in Conakry. The discovery was made on ultrasound of the first trimester of pregnancy and macroscopic examination of the placenta. One of the neonates was alive, a healthy female and the other was polymal formed with facial dysmorphism, omphalocele and sexual ambiguity, fresh stillborn. There was no maternal complication towards a gestational trophoblastic tumor (T.T.G) in both cases. Efforts must be made in the prevention of T.T.G. by screening for twin molar pregnancies with healthy fetuses on transvaginal ultrasound in the first trimester, the dosage of HCG in the face of unexplained metrorrhagia, macroscopic observation of the placenta after each delivery and biopsy sampling of any suspicious placenta.
Introduction
Complete moles with a coexisting fetus, evolving at term with spontaneous vaginal delivery, without fetal and maternal complications, are rare. Early diagnosis of this association leads in the majority of cases to termination of pregnancy on the one hand because of the frequency of triploidy and on the other hand because of the maternal risk and the possibility of progression to persistent trophoblastic disease [1]. We report two particular cases of twin molar deliveries at term without fetal complication and without progression to maternal gestational trophoblastic disease in the gynecology-obstetrics department of the Donka national hospital, the Teaching Hospital (C.H.U) of Conakry and in the maternity ward of the Jean Paul II hospital in Conakry.
Patients and Observations
Case 1
This was Mrs. D.F.B, aged 19, primigravida and primiparous, with no particular history, admitted while in labor at the gynecology- obstetrics department of Donka National Hospital, Conakry Teaching Hospital, with two results of ultrasound performed with a transparietal probe during her pregnancy. These results did not mention any notion of hydatidiform mole or associated congenital malformation. The pregnancy would have progressed normally until its term without maternal or fetal complications. It was only after the delivery of a fresh stillborn, polymalformed (with facial dysmorphism, omphalocele and sexual ambiguity) child, that the macroscopic examination of the placenta made it possible to make the diagnosis of presumptive mole twin by the presence of a normal placenta attached to a vesicular mass characteristic of a mole. The biopsy sample allowed the histological diagnosis of a complete mole. The post molar follow- up had been organized without maternal complication 61 days before the closure of the service for renovation, on October 5, 2015.
Case 2
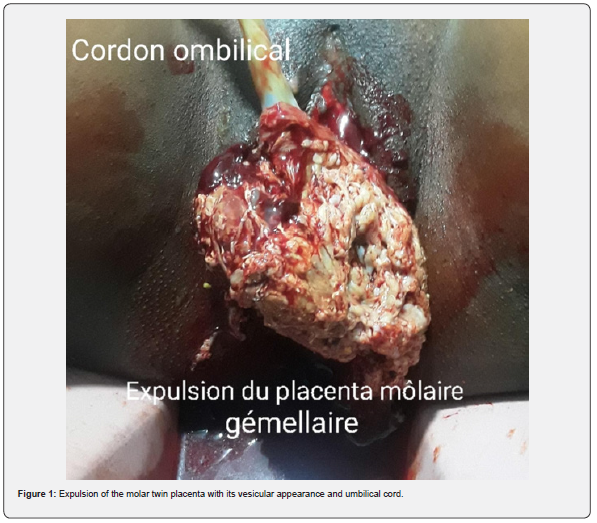
This was Mrs. H.C, seamstress, 30 years old, gravidity of 5 and parity of 5 including a twin birth and a laparotomy for ruptured ectopic pregnancy (GEU), who came on her own for a consultation for incoercible vomiting, physical asthenia on a menorrhea of 3 three months, June 19, 2020. The clinical examination had objectified a uterine height greater than the age of amenorrhea and dating ultrasound had made it possible to observe, intrauterine, a normal eutrophic fetus of 13 weeks – Amenorrhea (W.A) and a poorly vascularized heterogeneous multicystic mass. The beta HCG serum marker level was 16000IU/l. We had concluded a twin molar pregnancy and animated counseling on the interest of a medical termination of pregnancy to avoid the risks associated with serious maternal complications of trophoblastic tumor including choriocarcinoma. The couple, after a delay of two weeks, had opted to continue the pregnancy until its term. A pregnancy monitoring and childbirth preparation plan had been drawn up with the pregnant woman, whose morphological ultrasound at the 23rd W.A of the second trimester carried out on 03/09/2020, which had objectified a mass of 81 x 97 mm, in previa position. The pregnancy had progressed, without fetal and maternal complications, at 40 WA 2 days and ended with a vaginal delivery of a normal female child, alive and weighing 2830 grams. The woman had benefited from active management of the third stage of labor (TSLM) and digital uterine dissection to confirm the uterine cavity. Macroscopic examination of the adnexa had confirmed the presence of two separate placentas, joined together (Figure 1), one of which appeared normal and linked to the umbilical cord and had a histologically confirmed vesicular mass of “complete mole”. The planned post-molar follow-up was regular with progressive regression of the beta HCG level until negativity on the fortieth day of delivery without any clinical particularity on the closing date of January 31, 2021.
Discussion
The diagnosis of the association of a live fetus with a normal karyotype with a hydatidiform mole is often difficult, especially in the absence of revealing clinical signs [2,3]. The diagnostic modalities of molar twin pregnancy associating a complete mole with a healthy fetus were different due to the early ultrasound detection in the first trimester and the observation of the placenta. The lack of diagnosis of the coexisting mole during pregnancy despite the two ultrasound examinations in the first case would be linked to the age of the ultrasound scanners, which are often second-hand, the technique used (endovaginal in the first trimester or transparietal) and of the operator’s experience in the first observation. Early ultrasound detection made it possible to develop a follow-up plan for pregnancy, childbirth and postpartum in the second case. In the event of a twin pregnancy associating a live fetus and a molar pregnancy, the pregnancy can be continued until term if the patient wishes after having been informed of the risks and the most frequently reported complications (hemorrhages, late miscarriage, fetal death in utero and preeclampsia) [3]. Evacuation of the pregnancy is required only in cases of fetal anomalies or deterioration of the maternal condition [4]. The probability of obtaining a live birth varies between 16 and 56% [5] or 16 and 60% [4] deliveries. The continuation of the pregnancy is against payment given the risks of immediate and distant maternal complications. Close monitoring of the mother and fetus can help achieve a favorable outcome [4]. We accepted monitoring despite the maternal risks for one of our two pregnant women. The two pregnancies resulted spontaneously in the normal delivery at term of a healthy living fetus and another which would have succumbed to its multiple malformations per partum. The most feared complication is progression to gestational trophoblastic disease [1]. The diagnosis of postmolar Gestational Trophoblastic Tumor (G.G.T.) can be made according to criteria such as the persistence of h.C.G detectable more than 6 months after uterine evacuation and the histological diagnosis of choriocarcinoma [5]. According to Ikram Boubess et al., who adopted termination of two of these pregnancies, one remotely progressed to an invasive mole [6]. Regular monitoring of h.C.G levels throughout pregnancy and the postpartum period is necessary to detect GTN [7]. For Suksai M et al., a pregnancy with an initial serum h.C.G level of less than 400,000m.U.I/ml is a good candidate for the continuation of the pregnancy and the achievement of fetal viability [8]. The incidence of post-molar GTN is higher in twin pregnancies combining a complete hydatidiform mole (CHM) and a normal fetus than in single CHM [9].
Conclusion
Spontaneous evolution of the association of molar pregnancy with a live-to-term fetus, without immediate fetal and maternal complications, is possible. The most formidable complication, gestational trophoblastic tumor, choriocarcinoma, was not observed during the study period. The prevention of this complication requires the training of providers in endovaginal ultrasound, its systematic practice in the first trimester of pregnancy, ultrasound and biological monitoring of suspected cases during pregnancy, systematic macroscopic examination of the placenta with biopsy of cases suspect for histological confirmation.
To Know More About Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access
Journals Please click on: https://juniperpublishers.com/index.php


Comments
Post a Comment