Initial Blood Sugar Levels in Allegedly Diabetic Police Detainees in South London over a 4 Year Period
Journal of Forensic Sciences & Criminal Investigation
Authored by: *Robert Bruce-Chwatt
Initial Blood Sugar Levels in Allegedly Diabetic Police Detainees in South London over a 4 Year Period
*Robert Bruce-Chwatt
Senior FME to Metropolitan Police, London
Submission: March 08, 2016; Published: April 20, 2016
*Corresponding author: Robert Bruce-Chwatt MBBS, MFTM DFFP, (pt1 DMJ), Senior FME to Metropolitan Police, London, Tel: 0044-0-208-940-9781; Email:: Robert@bruce-chwatt.fsnet.co.uk
How to cite this article: Robert B-C. Initial Blood Sugar Levels in Allegedly Diabetic Police Detainees in South London over a 4 Year Period. J Forensic Sci & Criminal Inves. 2016; 1(1): 555554. DOI: 10.19080/JFSCI.2016.01.555554
Abstract
When questioned as part of the routine risk assessment by the custody sergeant, when prisoners are bought to a police station, some may then falsely declare themselves to be ill or on medication for chronic illnesses. This results in a referral to either the custody nurse or the duty FME. The motives for these false allegations are varied, but the risks of giving such false information especially relating to type, dosage and frequency of medication are potentially fatal. In those who have declared themselves to be diabetic it has occasionally been felt that in retrospect not all of them were being truthful. A review has been done of the results over a 4-year period of those who had declared themselves to be diabetic and agreed to have a blood test done. This has shown that 65% have a blood sugar level in the normal range on initial testing. The importance of repeated blood sugars during their detention is stressed for monitoring and as part of the handover to the next clinician. It is vital that these results be logged in the official custody record for later reference. Incidents have occurred when diabetics have pretended to inject their insulin in the misguided anticipation of a transfer to hospital when they become ill. All dosages of insulin should be double checked and self administration by the patient very carefully observed. The treatment of hypoglycemia using easily available and measured sugar portions from high street coffee shops is also discussed from a practical and common sense approach that is so often required in custodial medicine.
Keywords: Diabetic; Hypoglycemia; False allegations; Blood sugar level; Insulin; Custodial medicine
Introduction
The announcement on 17th August 2015 by Diabetes UK of the 60% increase of diabetes in the last ten years, mainly (90%) Type 2 and linked to poor diet with high sugar levels and consequent obesity, is of concern. The cost in terms of morbidity and mortality, as well as financial, is huge accounting for 10% of the £10 billion NHS expenditure on diabetes being spent on medication alone. Vascular complications from diabetes result in 135 foot amputations every week. Recent figures for the UK show that two thirds of all adults were overweight with a quarter being clinically obese and that on in 12 British adults now has diabetes. In 2015 more than 120,000 patients were newly diagnosed with diabetes [1]. This rise is also reflected in those members of the general public that find themselves in police custody, although that may be a conservative figure given that those who find themselves in custody are more often that not those in the lower income brackets and who tend to eat fast foods with a high sugar content. There is also of course the unknown number of people who have diabetes, but have yet to be diagnosed.
Although admittedly anecdotal, it is a well accepted premise, that prisoners in any form of custodial situation and when in a medical consultation with a doctor or nurse, may well declare illnesses that do not exist, exaggerate those that do or allege symptoms and conditions that are false, along with a past medical history that is both confused and/or deliberately untrue. There has been a number of papers published dealing with the medical and mental assessment of police detainees, their clinical care and medication [2-4]. It is then a regrettable fact that doctors working with such patients in a custodial milieu should be very cautious about accepting patient information given by detainees at face value. Information and awareness about diabetes is increasing in the general population and subsequent GP visits, as mentioned earlier, have resulted in the recent rise in the diagnosis of all types of this illness in the UK. Conversely it is often misperceived, and thus sometimes falsely declared by prisoners, as a dangerous illness, which, if handled sensibly, it is not. If diabetes is declared the doctor should always suggest that the patient consent to a base line capillary blood sugar level at the initial consultation and again subsequently to show a pattern or of if treatment is clinically indicated. Any suggestion of treatment with tablets or insulin without doing a blood sugar is clearly negligent either way. In such circumstances the use of a medical template as an aide-memoire is often very helpful [5]. The usual clinical targets for diabetics is to aim for the range of a non-diabetic. These are blood sugar levels two hours after food of 3.9 – 8.0 mmol/L and levels before food of 3.5 – 5.5 mmol/L. However, used here as a rule of thumb in custodial situations, a “normal” range of 4.0 mmol/L to 10.0 mmol/L has been applied for those fit to detain.
Case I: As mentioned earlier, forensic medical examiners who take all they are told at face value do themselves no favours and may risk their patient’s well-being if they treat them on this basis during such consultations. The philosopher’s “middle way” is the best approach; write everything down and then decide on clinical signs and clinical history what is or may be credible. In the case of declared diabetes; the patient being offered a capillary blood test to allow a reasoned clinical decision to be made in relation to management and treatment if required. Responses to clinical questions on their diabetes such as: “Insulin-insulin”, “10mls twice a day “or” the nurse does all my injections” are unlikely to impress and have all been heard. The occasional outright refusal to allow a blood test does not necessarily mean they are not diabetic, but is suggestive of this being the case. The excuse of a needle allergy, when it is of course a phobia not an allergy, is common, but noting tattoos or body piercings and then commenting on this makes this less likely to be pursued. It is dangerous, however, to discount the possibility entirely; in clinical medicine never say never and never say always. The importance of the initial base line figure, when time and date are recorded in the custody record, is that this allows sequential monitoring by following colleagues of the blood sugar in a case when a true diabetic just happened to have a blood sugar in the normal range at that time. Some doctors do not record the blood sugar in the custody record on the grounds of patient confidentiality; this is misinterpretation of ethics, unhelpful and foolish. Persistent normal levels over several hours, when measured and recorded in the custody record by subsequent duty doctors, often persuades the patient to admit that he or she is not diabetic. One detainee gave an excellent history and very believable insulin figures, but when later challenged over repeated normal blood sugars admitted he was not diabetic, but that his mother was and he regularly helped her as she had very poor eye-sight. Such a history is a very dangerous thing to allege with the risk of being believed and then of accepting treatment rather than admit lying or in the hope of being hospitalised. The scenario of becoming unconscious for another reason and then being mismanaged, on the basis of the history given, is even worse. For one prisoner the good news was that he was not an insulin dependent diabetic; the bad news that he would not be going to hospital, as he has angrily and volubly demanded, with a chance of escape. In the end it is all about the patient’s safety in custody.
Apart from their diabetes, medication that they may have been prescribed for other conditions is often taken in a poorly compliant manner; when they remember or can be bothered or not at all. It is of vital importance to ask when they last took any medication as this may have been weeks, even months ago even though they will have told you they are “on it”. Such custodial patients may also be abusing a variety of illegal drugs including heroin, crack and cannabis. The effects on metabolic rate of these depressants and stimulants can be considerable and clinical histories are sometimes bizarre. Often heroin and crack are abused together either as a 50-50 melange “speed ball” if injected or as a “snowball” if smoked which further confuses matters rather than evening things out. The concomitant use of alcohol, often including a dependency, is also a problem. The current use of the word “issue” instead of “problem” is bizarre and unhelpful. Alcohol, though itself a body carbohydrate load, requires energy to be metabolised and excess alcohol may in fact lower the available blood sugar. The smell of ketones on the breath of a hypoglycaemic insulin dependent diabetic may be mistaken for the smell of ethanol, when in conjunction with apparently intoxicated behaviour. If missed this may well result in tragically fatal results and a death in custody when they are put back in a cell to “sober up”.
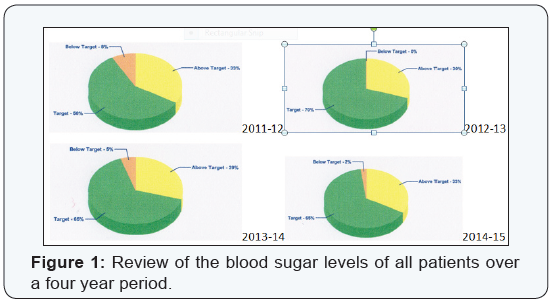
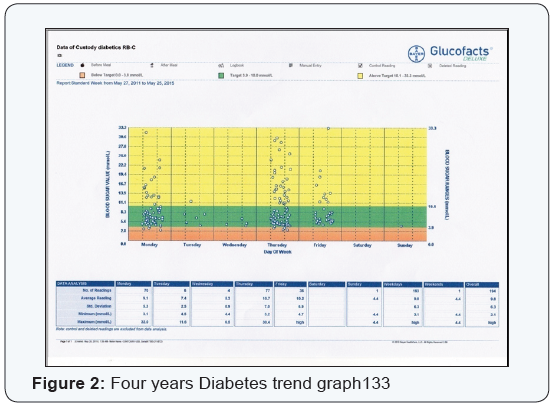
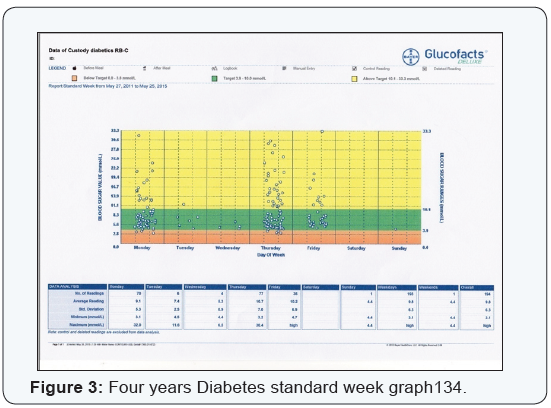
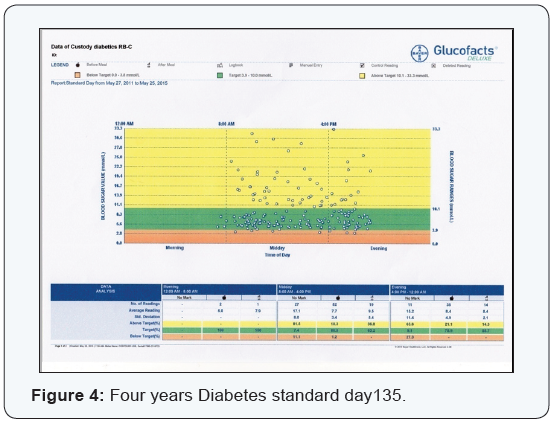
This has been the experience of the author, but thankfully without the death, when an elderly IDD insisted that he was not diabetic and refused to have a blood test. A blood test, taken without his consent, revealed a blood sugar of 2.2mmol/L. This decision, though technically in law a common assault by the author, proved both life saving for the patient and profession saving for the FME. When given sugar orally and his blood sugar level had returned to normal, the patient denied all memory of the conversation and could not understand why he had denied being diabetic. In retrospect this was most probably a state of incipient delirium prior to him losing consciousness as his blood sugar became critical. Conversely a genuine IDD, who had been suitably and fully assessed by the author feigned injecting his insulin and managed, unseen, to squirt it on the wall instead. He then demanded, not unreasonably, to be fed saying he was very hungry and ended up in hospital for three days to be sorted out, this being exactly what he had wanted. Following these incidents a review of the blood sugar levels of all patients seen over a four year period, who had declared themselves to be diabetic, was done (Figures 1-4). This was for ad hoc FME duty periods of 06:30 to 18:30 hours between the 27th May 2011 to 26th May 2015. Since the Glucometer used has a memory and applies time and date stamps this was possible.
Method
The two samples of white sugar from each source were weighed unopened on a set of Fuzion FZ-350 electronic scales [6] bought by the author from the somewhat bemused owner of the local “bong-shop” or “head shop” in Brixton, where drugs paraphernalia are sold. The average weight for all the sample sachets of white sugar was 2.84 grams with Costa, Whole Foods and Prêt having the best regularity in weight. Perhaps it is also now high time for any suppliers of these sugar portions to give the weight in grams on the packaging? This should also be the case for all Airline sugar packs, so that when the tannoy call goes out for a physician to assist during an in-flight medical crisis, he or she is aware of the amounts and can calculate accordingly for treating a diabetic hypoglycaemia. On a recent Swissair flight the author was provided with both straws (5.2gm and 5.0gm) and sachets (4.4gm and 4.5gm); the respective weights being ascertained on returning home.
Glucometer
All measurements were done using a Bayer Contour-USB blood glucose meter with Bayer Contour® test strips [7] The Contour® meter provides a quantitative measurement of glucose in a drop of blood from 0.6 mmol/L to 33.3 mmol/L and with a mini LCD display is default programmed to visually suggests seeking medical assistance if below 2.8 mmol/L or above 13.9 mmol/L. The reading is based on measuring the electrical current produced by the reaction of glucose with FAD glucose dehydrogenase and potassium ferricyanide; the electrical current produced being proportionate to the amount of glucose present in the measured capillary sample. The meter, with a USB connection, has the advantage of being programmable on a PC, with default settings being able to be changed and is rechargeable at the same time. It also allows a number of extra bits of information to be keyed in when capillary blood sugar level is measured. The excellent internal program on Java script also automatically produced the four detailed charts used to illustrate this paper. The price of the test strips are £25.00 for 50, giving a 50p cost each time.
Treatment of hypoglycaemia with oral sugar
It should always be remembered that a low blood sugar is more critical than a high blood sugar and the author has seen patients with levels of 30 mmol/L and above who had no idea, until told, that their levels were that high. In the absence of a Glucometer or when having run out of test strips or the machine does not work and a diabetic patient has said that they: “don’t feel very clever” and is clearly unwell, then giving some sugar whilst waiting for an ambulance is a sensible and possibly lifesaving decision. Some doctors use the “Rule of 15” when treating hypoglycaemia, but I do not advocate it for reasons of the delay. The old-style “sliding scale” is often the best and the one used here, but as a clinical decision it is that of the treating physician, albeit after discussion with the patient who will often, after many years, knows a great deal about their own diabetes and, if honest and sensible, can do much to help manage their illness during a difficult and stressful period.
With the closure of many police station canteens and the current, and probably continued absence, presumably for financial reasons, of the old Metropolitan Police Catering Services white sugar pack (3.8gm) as a measured and easily available source of sugar, the author has found the portions or “straws” of sugar available at the many UK High Street coffee shops invaluable to have in a jacket pocket; but never, of course, stored with the Glucometer. White sugar contains 3.96 calories per gram and has a very consistent granule size whilst brown sugar has a higher water content and contains 3.73 calories per gram and the granules tend to be a little smaller in size. Thus gram for gram, white sugar has more calories, but measure for measure, brown sugar will have more calories. Only white sugar was used in this study and was given by the sublingual route with the inevitable dissolved portion being gradually swallowed. (Table 1)
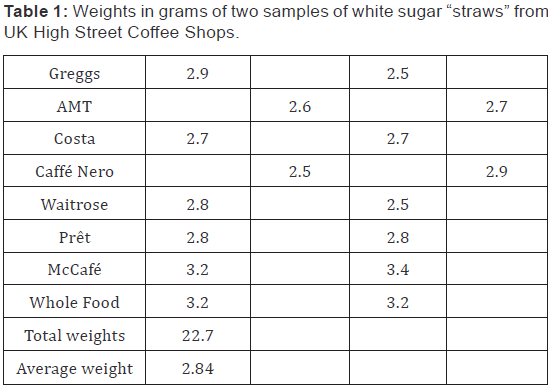
With sublingual administration the sugar is in contact with the mucous membrane under the tongue and diffuses through it. The connective tissue under the epithelium contains a profusion of capillaries; the sugar diffuses into them and rapidly enters the venous circulation. It is thus direct, rapid and is unaltered by the enzymes present in the saliva (the sero-mucous saliva from the sub mandibular glands being stimulated by the presence of the sugar) before entering the blood stream and becoming available for use. Conversely sugar absorbed in the intestines is much delayed and subject to first-pass metabolism in the liver before becoming available in the general circulation. The single white sugar portions were obtained from Greggs, AMT, Costa, Nero, Waitrose, Prêt, McCafé and Whole Foods and survey of the weights in grams of “straws” available is seen in the chart below:
Physiology
How much will one gram of refined white sugar raise the blood sugar of a non-diabetic? Well, it depends on weight, since weight is part fluid volume. If they weigh, in these modern times the now near mythical 64 kilos or 140lbs, then one gram will raise it by around 0.22 mmol/L; if they weigh twice that much, it will only raise it half as much and vice versa if they weigh 32kilos or 70lbs. The maths of dilution remains the same though BMIs of most of our patients have risen considerably. The 64 kilo/140 pound insulin dependent diabetic needing urgent treatment for hypoglycaemia has an “advantage” as they are not producing insulin and cannot offset the added glucose. So 1 gram of sugar will raise their blood sugar by about 0.22 mmol/L regardless of what their blood sugar was before. Treatment with glucagon injection is available in the medical cabinet at all UK Met police custody suites if the detainee is unconscious, but speed may be of the essence and sugar is much simpler answer whilst awaiting the ambulance. If of course, they are still conscious and capable of cooperation. The need for them to go to A&E once their blood sugar level is reasonable remains debatable, but today’s doctors have become so risk averse, especially in custodial medicine, that such transfers are becoming almost inevitable.
Result
This showed that over a four year period 65% of those tested had a blood sugar within the normal range with 4% being below target and 31% being above the target range. It is interesting to note that in the first year 24 blood glucose levels were measured of which 58% were in target:; in the 2nd year 27 of which 70% were in target, in the 3rd year 55 of which 65% were in target and in the last year 88 of which again 65% were in target. There has been a marked increase in the numbers of diabetics in the general population, most probably due to the increase in obesity and this appears to be mirrored in the custodial population especially over the last two years when in year three it doubled and then when it increased again by 60 % in year four. However the percentage of in target blood levels did not increase and in fact, pro rata, has therefore decreased in the last year.
Discussion
All the patients had declared themselves to be diabetic, hence the measurement of an initial blood sugar. A larger and more complex met-analysis could be done relating also to age, sex, time, insulin dependence, tablet dependence or diet controlled, but in this initial study the question of initial and consequent blood sugar levels, following police arrest of an alleged diabetic, was all that was considered. This showed that 65% of the patients presenting as self-declared diabetics had a normal blood sugar at their first custodial assessment. The caveat should still remain that this measurement should be repeated after a suitable time to attempt confirm or deny the initial information and allowing treatment and monitoring if abnormal. In the past we often worried more about diabetics; perhaps after viewing these results those concerns should be more concentrated on the increasing numbers of alcohol dependent detainees withdrawing whilst in custody and the risks of fitting and possible death.
To know more about: Juniper Publishers - Opinion Stage

Comments
Post a Comment