Silent Somatotropic Adenoma and Pregnancy: About A Case-Juniper Publishers
Global Journal of Reproductive Medicine Juniper Publishers
Authored by: Sara askaoui*Introduction
Silent somatotropic adenomas correspond to a rare entity. Their diagnosis is based on screening by the systematic determination of GH under oral glucose tolerance test (OGTT) and insulin growth factor 1 or the immunohistochemical study, in the absence of clinical signs of acromegaly [1,2]. Pregnancy in acromegalic women is an exception. Data from the literature report the absence of fetal malformation, an increase in adenomatous volume that is rarely symptomatic, a possible risk of gestational diabetes and gestational hypertension in women not controlled by pre-pregnancy drug therapy [3,4]. Variations in somatotropic function have rarely been studied. The aim of this work is to report the case of pregnancy in a patient followed for a silent somatotropic adenoma.
Case Report
A 33-year-old patient who was seen for secondary amenorrhea with anamnesis: asthenia, frontal headache, and galactorrhea. The clinical examination did not indicate a dysmorphic syndrome, noted the presence of multipored galactorrhea caused. The results of the hypophysiogram were as follows:
• Prolactin: 153 ng / ml,
• TSHus: 1.2 mUI/l, T4L: 9pmol/l (12-22),
• FSH: 1.3 UI/L, LH: 0,9 UI/L and
• Oestradiol: 9pmol/l.
The somatotropic axis has not been explored.
Pituitary magnetic resonance imagery (MRI) revealed a pituitary macro-adenoma of 18 *13*16 mm, repressing the optic chiasm and cavernous sinuses (Figure 1), with the visual field: an enlargement of the blind spot with an amputation of the infero-nasal area of the left eye. The adenoma was treated by cabergoline 10mg per week for one year with substitution of thyrotropic deficiency. The evolution at one year was marked by the persistence of the latter, with a control prolactinemia at 0,22 ng / ml. The controlled pituitary MRI noted an increase (by 17%) of the tumor volume: 21 * 19 * 15.3mm, with a visual field always altered.

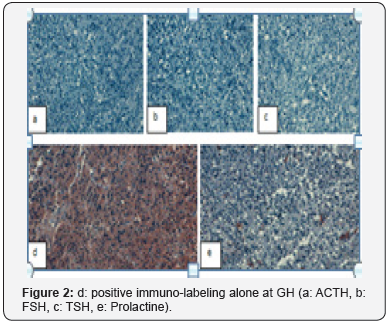
An echo-heart was requested as part of the follow-up, further, to increase the dose of cabergoline which revealed the presence of an average tricuspid insufficiency. The latter was declared at the pharmacovigilance center, then, the indication for transphenoidal surgery was raised. The consistency of the tumor was fibrous and haemorrhagic making it impossible to extract. Immunohistochemical analysis returned to a typical somatotropic adenoma (Ki 67 <3%, P53 not done) (Figure 2).
Pituitary MRI for control at 3 months post-operative showed constant tumor volume with some necrosis areas with IGF1 at 131ug/l (112-300). The patient was seen after being pregnant at 19 weeks; whose follow-up did not indicate gestational diabetes, nor gravid arterial hypertension, nor signs of intracranial hypertension, nor fetal malformation. Radiological control at 3 months of the postpartum, showed the stability of the tumoral volume with a level of IGF1 always normal. Surgical revision was indicated with supplemental treatment with somatostatin analogues.
Discussion
The somatotropic adenomas are often identified because of the clinical consequences they cause (dysmorphism). Occasional cases of subclinical adenomas have been described in the literature, where only pathological examination reveals a positive immuno-labeling for GH (somatotropic, cortico-somatotropic and somato-thyrotropic) [5].
Their frequency is poorly studied [6], because in the absence of immune-histochemical study, a nonfunctional adenoma is concluded and IGF1 is not carried out as part of the follow-up; all this leads to a delay in diagnosis, which later gives rise to dysmorphism with the various complications of hypersecretion of GH [7]. For this, a preoperative evaluation of the concentrations of GH / OGTT and IGF-1 is of interest, in addition to the complete histopathological analysis: immunohistochemistry of GH, prolactine, expression of somatostatin receptors and evaluation of proliferation (number of mitoses, Ki-67 index and p53 expression). The treatment of this type of adenoma is initially based on surgery, then somatostatin analogues and lastly on temozolamide and radiotherapy in case of signs of aggression [8,9].
Pregnancies in these patients treated for acromegaly are often not accompanied by obstetric or fetal complications, but a maternal follow-up is necessary in order to diagnose gravid hypertension and gestational diabetes. On the other hand, a clinical monitoring of pituitary tumor syndrome is necessary in women with nonoperated GH macroadenoma before pregnancy [10].
Conclusion
Silent somatotropic adenoma is a distinct entity from the usual cases of acromegaly, as it may be a beginning of the disease, or a benign aspect of the disease. The systematic implementation of the GH / OGTT and IGF1 preoperatively associated with the immunohistochemical study is of great interest, allowing the screening of this entity and ensuring appropriate monitoring. Clinical monitoring of pituitary tumor syndrome is necessary in pregnant women with non-operated GH macroadenoma.


Comments
Post a Comment