Osteoporosis and Fragility Fracture in Pregnancy A Case Report-Juniper Publishers
Global Journal of Reproductive
Medicine Juniper
Publishers
Authored by: Susana Pereira*Introduction
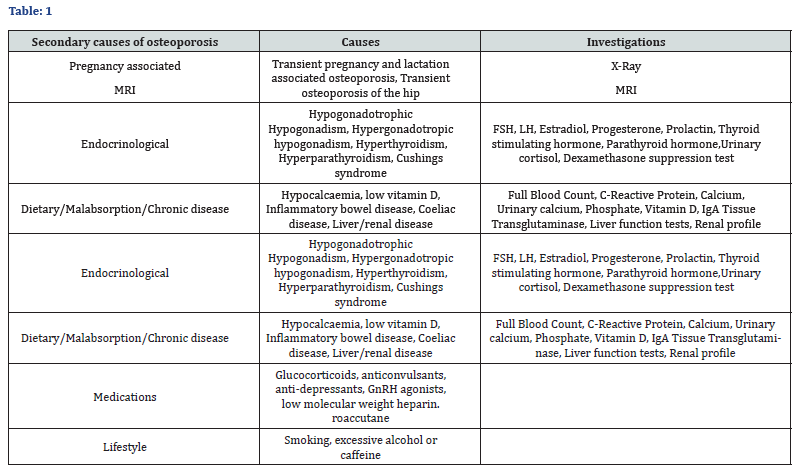
Osteoporosis is characterised by low bone mass secondary to inadequate acquisition of peak bone mass and/or increased bone loss. Osteoblastic and osteoclastic imbalances result in reduced bone mineral density (BMD), disrupting bone’s normal microarchitecture and predisposing to fragility fracture [1]. The prevalence of osteoporosis in premenopausal women is approximately 0.5%. Where there are no secondary causes of osteoporosis found (Table 1), it is termed idiopathic osteoporosis. Pregnancy and lactation are thought to cause secondary osteoporosis (PLO) [2]. The overall incidence of PLO remains largely unknown due to a lack of large scale population based data in this area [3]. Little is known about managing pregnancy induced BMD loss superimposed on pre-existing osteoporosis. This case illustrates the challenges faced in balancing the obstetric, medical and orthopaedic needs of such a patient.
Case Report
A 24-year-old non-smoking primagravida was referred for obstetric review at 13 weeks gestation having sustained a previous atraumatic left neck of femur fracture (conservatively managed). She had prior multiple low impact fractures to both wrists, ankles and left foot. Dual-Energy X-Ray Absorptiometry (DEXA) scanning showed Lumbar spine scores: T –2.7, Z –2.7, Left hip: T –2.3, Z -2.3, Left femoral neck: T-3, Z-3. Lumbar spine and left femoral neck T scores showed marked osteoporosis, whilst Z scores showed low BMD. Investigations for secondary osteoporosis were all negative, including bone biopsy (Table 1).
Risk factors for osteoporosis included a six-month period of amenorrhoea secondary to anorexia nervosa and six months of Roaccutane use. Pregnancy was uneventful and following obstetric and orthopaedic review vaginal delivery was recommended, with advice to limit lactation to 3 months postpartum. At 34 weeks gestation the patient presented with progressive right hip pain aggravated by weight bearing. MRI revealed a new right midsuperior pubic ramus stress fracture. Orthopaedic review advised minimal mobilisation with crutches for support. The patient opted for elective caesarean section under regional anaesthesia at 38 weeks, despite no formal contraindication for vaginal delivery. Rheumatologists advised a year long interval after ceasing lactation before conceiving again to allow bone recovery.
Discussion
PLO is thought to arise from a combination of factors. Karlson et al. [3] attributed pregnancy BMD loss to high fetal calcium transfer. Postnatally, raised parathyroid and prolactin levels suppressing the hypotholamaic-pituitary axis, reduced oestrogen production, decreased maternal weight reducing skeletal loading and breast milk calcium losses were suggested causes of BMD loss.
Paucity of longitudinal studies between BMD and fracture incidence in premenopausal women, means diagnosis of premenopausal diagnosis remains a challenge [2]. DEXA findings alone cannot be used to make a diagnosis in premenopausal patients and secondary causes must be excluded. Z-scores <-2.0 typically indicate low BMD, but if used in isolation may not correctly diagnose osteoporosis, as peak bone mass is not reached until 30 years of age [4]. Hence, Z-scores matched for age, sex and ethnicity are recommended for measuring BMD in premenopausal women versus T-scores [5].
Fractures are a cause of significant morbidity. Outside of pregnancy they are related to an increased risk of venous thromboembolism (particularly in lower limb/pelvic fractures) [6], depression [7], as well as chronic pain [8]. Those with premenopausal fractures have a 35% increased risk of postmenopausal fractures [9]. During pregnancy, the mainstay of treatment for severe osteoporosis is through calcium, vitamin D supplementation, falls prevention, physiotherapy and lifestyle changes. Calcium supplementation has been shown to be ineffective in preventing bone loss in lactation [10]; weight bearing exercises are less practical in the peripartum period and as most women cease alcohol and smoking in pregnancy, these interventions are likely to have minimal benefit. We have therefore reviewed the literature for alternative therapies.
Bisphosphonates act as potent osteoclastic inhibitors [11]. Although bisphosphonates are approved by the FDA for glucocorticoid-induced osteoporosis in certain pre-menopausal women, they are generally not recommended due to the risk of embryo-fetal toxicity [12]. Rodent studies have shown neonatal skeletal abnormalities and low birthweight [13]. Overall, use in premenopausal women remains contentious due to their long half-life within bone - in excess of ten years [14]. Stathopoulos et al. [15] reviewed 78 cases of fetuses whose mothers had been exposed to bisphosphonates either prior to or during pregnancy. A few cases reported shortened gestational age, low neonatal birth weight and transient hypocalcaemia, but overall none developed serious adverse events. Stathopoulos et al. [15] concluded that although the safety of bisphosphonates required more evidence, they advocated use of bisphosphonates in women of reproductive age as long as IV bisphosphonate was used (with use ceased 6 months prior to conception) and maternal and neonatal calcium levels were monitored.
Recombinant Human Parathyroid Hormone (hPTH) is an anabolic agent used to treat refractory osteoporosis by stimulating osteoblasts [3]. In a case series by Choe et al. [16] three women with PLO and vertebral fractures showed a reduction in pain and no further need for orthosis within 1-5 months of treatment, an improved BMD by 18 months of therapy and no adverse effects on subsequent pregnancies. Clinical trials have not yet been performed in premenopausal women after rodent studies raised concerns about fetal skeletal abnormalities including osteosarcoma [17,18]. However, with its short half-life (1 hour) Choe et al. [16] recommended hPTH as potentially successful for PLO patients with pain and multiple vertebral fractures. One report from Israel describes the use of PTH in pregnancy for hyperparathyroidism without any adverse fetal outcomes [19].
Denosumab, is a monoclonal anti-receptor antibody which decreases osteoclastic activity [20]. Unlike bisphosphonates, it has a shorter half-life and no skeletal accumulation [21,22]. However, in animal studies Denosumab was attributed to increased neonatal mortality and reduced growth. Drug related changes were also found in neonatal lymph nodes and bones [23]. In a single case of inadvertent Denosumab use one week into pregnancy, no adverse fetal or maternal outcomes were report [24].
Postpartum Management
Lactation is thought to cause bone losses of 3-10%, with pregnancy causing losses of 3-5% [3]. A direct relationship is thought to exist between the duration of lactation and degree of BMD reduction. Recovery of BMD is thought to take 6-12months after cessation of breastfeeding [5]. Discussion with the patient should occur to balance breast feeding benefits with risk of lactational osteoporosis.

Comments
Post a Comment