Unintentional Acute Carbon Monoxide Poisoning During Pregnancy: Five Years of Experience in Bordeaux-Juniper Publishers
Global Journal of Reproductive Medicine Juniper Publishers
Authored by: Jose Rajaonarison*
Introduction
Carbon monoxide (CO) poisoning is a common intoxication found in France. It causes serious outcomes on population with a mortality rate of 0,31/100000 in some areas of France [1], a sudden lethality for 1,26% [2], and neurological sequelae that might be severe. In France, 5,4% of victims are pregnant women [3]. The rate of fetal mortality due to CO poisoning during a pregnancy can reach 19 to 24% [4]. The physiopathological suggestions had proved that a foetus is more susceptible regarding of intensity and duration of exposure than a mother. Although various studies had brought light on how to understand physiopathologies, diagnosis, therapy principle; the frequency of neurological sequelae, pronostic factors, the fetal prognosis of a CO exposure during pregnancy and the monitoring system of victims remain in shade. Practices diverge on how to prescribe an hyperbaric oxygen therapy.
The following study aims to describe maternal and fetal complications of CO poisoning during pregnancy. From the obtained results, the prescription of an HBO therapy, maternal sequelae and fetal prognosis will be discussed.
Materials and Method
A retrospective and descriptive study based on observation of patients was conducted. Women poisoned with carbon monoxide and admitted to hospital were included in the study. A list of patients was retrieved from the UCAIM (Unit of Coordination and Analysis of Medical information) data at the UHC (University Hospital Centre) of Bordeaux over 5 years and 6 months (from 01/01/2011 to 30/06/2016). Patients who did not deliver in Bordeaux or not having a filed telephone number were excluded from the investigation. Other patients who had delivered in other centres were contacted by phone calls to get informed on the evolution of the pregnancy and its outcomes. For each patient, the background of the poisoning was investigated (cause, duration of exposure, ambient concentration of CO), together with clinical and paraclinical manifestations, management (normobaric and hyperbaric oxygen therapies), the evolution of the pregnancy and all possible sequelae (Table 1-2).
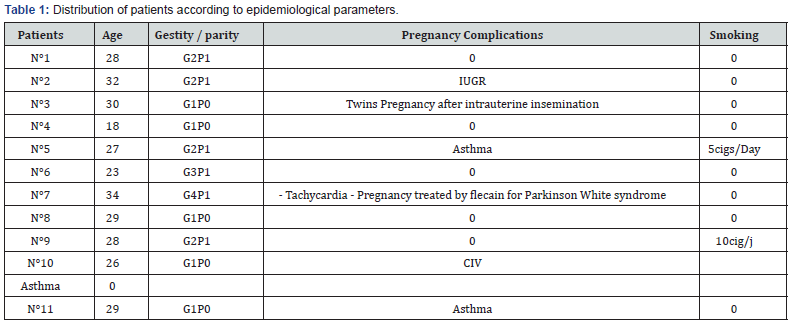
IUGR: Intra uterine growth retardation; IAC: husband’s sperm insemination; CIV: inter-ventricular communication.
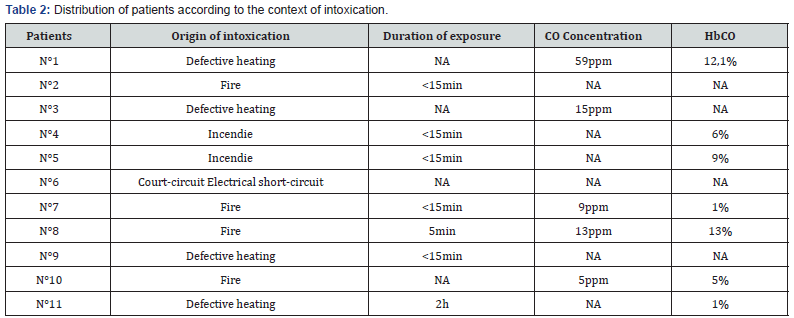
ppm: part per thousand.
Results
Data from the twenty four pregnant women were collected upon 248 cases of CO poisoning treated at the centre giving a rate of 9,67%. Eleven of them were completely monitored, the remaining (13cases) were not included in the study. The epidemiologies and features of the poisoning were respectively shown in table I and II. Eight women were asymptomatic and four others presented neurological symptoms as (headaches, dizziness, malaise, mild loss of consciousness, asthenia). Two of them have shown one with digestive signs (nausea, vomiting) and the other with asthenia. Obstetrical manifestations were illustrate on table III. An Electrocardiogram (ECG) performed on ten patients revealed that one of them had presented a right bundle block. Eight patients out of the eleven were treated with face fitted masked normobaric oxygen (NBO) at a flow rate of 15L/min before admission to hospital. The average time elapsed between the intoxication and the onset of an hyperbaric oxygen (HBO) treatment is of 11,75h with margins of 4 to 48h. The pressure used was of 1,5ATA (Atmosphere absolute) (9/11) and 2,5ATA (2/11). The duration of the HBO treatment depends on medical practitioners and according to the seriousness of cases; ranging from 115 min for 8 patients, 150min for two others and 190min for the last one. Perinatal complications were given on table IV. Within a period of 1 to 5 years one child out of 11 had two conditions of bronchiolitis before the age of two years (Table 3&4).
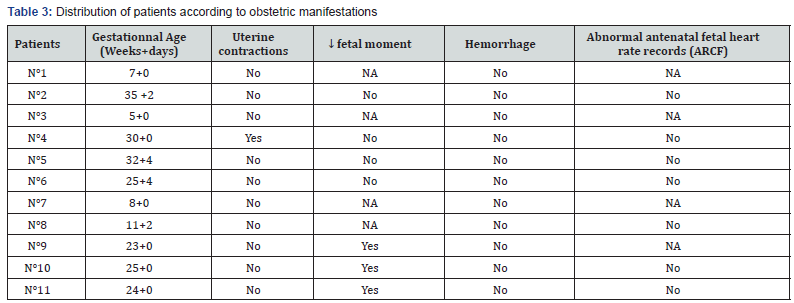
SA: Gestationnal age; MAF: actif fetal movement; ARCF: abnormal antenatal fetal heart rate records
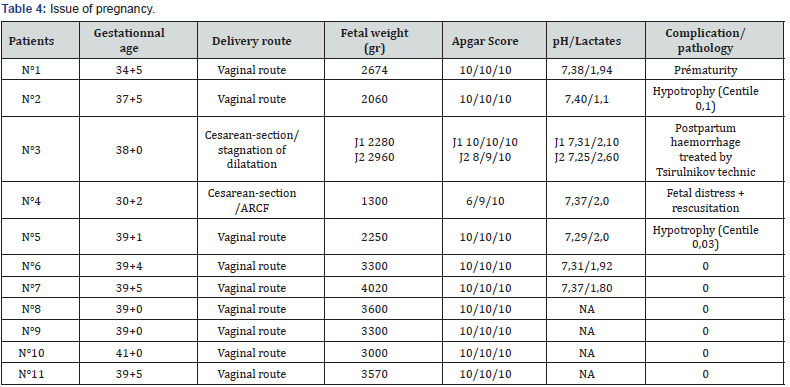
ARCF: abnormal antenatal fetal heart rate records, HPPI: Immediate postpartum haemorrhage.
Discussion
Carbon monoxide poisoning is the most familiar intoxication in France. The InVs (Institute of Health Surveillance) records 4000 cases per year but its incidence is underestimated for several reasons: reporting is not obligatory, intoxications from smokes are excluded from the declared case, and finally, since that gas is odourless and colorless and symptoms do not always appear, some cases of CO poisoning are often misdiagnosed [5]. In 2012, that condition was a very common hazard during pregnancy with a rate of 9,67% in Bordeaux [6], 8,5% [7], in United States and less frequent in northern France (5,4%) [3]. Among the reported causes were: fire, and faulty heating appliances which promote the spate of occurence during wintry season [8]. Practically, managing CO poisoning encounters issue in diagnosis. Its definition varies from one centre to another, ambient concentration is changing, and the duration of exposure is often unknown [6,9]. Clinical signs depend on the atmospheric concentration at the intoxication. In a range of 100-200ppm, headaches, nausea/vomitings, dizziness, asthenia and malaise appear. Within 300-500ppm, the patient may present polypnea, dyspnea, tachycardia, chest pains, and slight loss of consciousness. At 1000ppm, a convulsion, or a coma may take place. Between 2000-5000ppm death occurs in few minutes [10].
Minor disorders are noticed within 30 to 40% of cases [11], and more serious neurological manifestations occur in 1 to 4% [12]. During pregnancy, the most common signs are the reduction of the active fetal movement (3cases in this series), threat of a premature delivery (1case) but the poisoning may also be without symptoms. On a paraclinical basis, an Electrocardiogram displayed a common epicardial or endocardial ischemia [9]. In this series one case of bundle block was recorded. The plasmatic level of COHb correlates with the time elapsed after the hazard. Four patients were reported without that level. It was also the case of another study conducted at the same region in 2012, by Bernadet P and al. [6] all 76/252 cases were reported without the dosage. For a therapy management, a systematic treatment using NBO must be performed.
It was one of the basic therapy that is achieved at high flow rate (12-15L/min) using a face mask, and which should immediately be started at the premices of the accident. A regular check of the fetal heart beat is practiced for 1h [13], and the oxygen therapy must be continued for 16h or more if no improvement is observed or the hyperbaric oxygen is not available [14]. Eight patients out of the eleven had followed this treatment. Applying hyperbaric oxygen therapy (HBO) fastens the dissociation of COHb molecules, reduces its elimination half-life, rise the plasmatic concentration of oxygen and prevent formation of free radicals [15,16]. Its prescription during pregnancy is beneficial since it contributes to reduce the severity of the fetal injuries, the occurence of malformations and it was proved to be safe [17,18]. According to some authors, no significant difference of effectiveness is noticed when compared with a NBO therapy [19]. In literature the pressure used is usually of 2ATA for 120 min or 2,5 ATA for 90min [15].
Silverman RK, et al. [20] recommended another administration when maternal or fetal symptoms remain 12h after the first application. In Bordeaux, such session is systematically performed during pregnancy not regarding the severity of the intoxication. Oxygen pressure of 1,5ATA (9/11) for 115min is commonly used (8/11). A long record of the fetal heart beat is obligatory with a management of possible risk of premature delivery. One case was handled all along this study. A fetal hypoxia requiring an emergency caesarian section in one of the pregnant patient was the most frequent complication of this condition. It came out of a maternal hypoxia thanks to a high affinity of CO with the fetal haemoglobin, the delay of its elimination, and the misuse of oxygen by cells [3,4]. At a beginning of a pregnancy, malformations like microcephaly, dysgenesis of the telencephalon may occur within a second quaterly of brain injuries at the basal ganglia, brainstem, cerebellum and the spinal cord [15,21,22]. It resulted in hypotonia or even a cerebral palsy after delivery [23,24].
The absence of other causes of IUGR which involved two cases of this series allow us to realize that such growth restriction would come from the poisoning. Such complication had not yet been reported in literature. Moreover, the occurrence on one of the patient of a subchorionic hematoma could not be otherwise explained. Perinatal mortality associated to this intoxication can reach up to 36-67%. On the long run, no infant pathology was linked to a CO poisoning. The cases of broncholitis found on a child were not necessarily related to in utero CO exposure. As for maternal death, figure could attain 1,26% of the intoxicated. The prognosis is not different from that of non-pregnant women. No maternal death related to the poisoning was recorded during the study, however literature reported cases of adult losses during pregnancy [22]. Severe manifestations occurred in 1 to 4% of cases [12,25,26], leaving survivors with sequelae mainly depression, anxiety, or impaired cognitive ability resulting in disturbances at work [27].
The presence of a cardiac comorbidity (one woman has a VSD in this series), an abnormality of the Electrocardiogram (one case of right bundle block found on one patient) and various forms of poisoning (smokes from fire on 6 of the pregnant women) are part of the pronostic factors of the maternal mortality [28]. Neurological sequelae are feared when a loss of consciousness or an initial cerebellar syndrom [18,29], headaches, fainting or dizziness occurred, or failing a HBO therapy particularly when the blood level of COHb is >25% [15,30].
Conclusion
CO poisoning is not an exceptional condition at the centre of the study. A better management is obtained through a systematic oxygen therapy during pregnancy and it can improve the figure of prognosis. The French population still need to be informed of the risk of contracting home CO poisoning, its outcomes and management.

Comments
Post a Comment