Assessment of Postnatal Care Service Utilization and Associated Factors in Asella Town, Arsi Zone, Oromiya Regional State, Ethiopia-Juniper Publishers
Global Journal of Reproductive Medicin Juniper Publishers
Authored by: Legesse Tadesse *
Background
Post-natal care refers to the assistance given to the mother and the baby for a period of six weeks from the time of delivery. Maternal and child health are the major concern of public health organization and researchers throughout the world. Health education for mother is strategy many countries have adopted to improve maternal and child health. Yearly over half a million women encounter complication due to child birth and many die [1].
Post-natal services are the primary comprised of physiotherapy, physical examination, immunization, health education and family planning service [2]. Lack of care in this time period may result in death or disability as well as missed opportunities to promote healthy behavior, affecting woman, newborn and children. Post-natal care is regarded as one of the most important maternal health care services for the prevention of impairment and disability resulting from child birth [3].
Different studies in developed countries showed the factor which affects utilization of post-natal care are distance from health service, cost including direct fees and cost of transportation, drug and supplies; multiple demands on women’s time; women lack of power on decision making within the family; and poor quality of services including poor handling by health providers [4]. Half of all post-natal maternal death in Bangladesh occur during the first week after the baby is born, and the majority of these occurrences during the first 24 hours after child birth [5].
In a very poor countries and regions, such as those in sub- Saharan Africa only 5% of women receive post-natal care. In Ethiopia, factors associated to utilization of PNC service have been the major cause of maternal and infant death for majority of people, especially for those having low income. Therefore, it is important to assess the factor that cause underutilization of postnatal care service [6].
Statement of the problem
Approximately 80% of maternal death globally occur due to hemorrhage, sepsis, unsafe induced abortion, hypertensive disorder of pregnancy and obstructed labor [7]. These deaths are unjust and can be avoided with key health interventions, like provision of ANC and medically assisted delivery [8]. The emphasis on two out of eight critical united nation millennium development goals, that is reducing under five mortality by 2/3, between 1990 and 2015 and reducing maternal mortality ratio by ¾ between 1990 and 2015 epitomize of the relevance of indicator sign global efforts towards human development [9]. A fully functioning mother-baby package intervention has been estimated to have post-natal cumulative effect of averting 75%-85% of maternal death in developing countries [10].
A woman living in sub-Saharan Africa high chance of dying in pregnancy, child birth and after child birth [11]. Post-natal service are also among the strategies aimed at preventing the onset of physical and mental impairments among women who have delivered [12]. Nearly 4.7 million mothers, newborns, and children die each year in sub-Saharan Africa: 265,000 mothers die due to complications of pregnancy and childbirth and 3,192,000 children, who survived their first month of life, die before their fifth birthday [13]. 1,208,000 babies die before they reach one month of age [14]; this toll of more than 13,000 deaths per day accounts for half of the world’s maternal and child deaths. In addition, an estimated 880,000 babies are stillborn in sub-Saharan Africa and remain invisible on the policy agenda [15].
Despite remarkable progress to reduce mortality of children under 5 years of age in Ethiopia, little change has occurred in neonatal mortality, which accounts for 42% of all under-5 deaths. The 2000 [16], 2005 [17], 2011 [18] and 2016 [19], Ethiopian Demographic and Health Surveys (EDHS) reported neonatal mortality rates of 49, 39, 37 and 35 per 1000 live births, respectively. The decline in neonatal mortality rates by 24% over 11 years is substantially less than the decline in infant (39%) and child (60%) mortality over the same period.
Use of maternal and newborn health care services is low in Ethiopia. According to the 2016 EDHS, only 62.4% of women who gave birth in the 5 years preceding the survey received any antenatal care from a skilled provider (eg, physician, midwife, nurse), and 9% received antenatal care from a health extension worker. Only 10% of women gave birth in a health facility or with a skilled birth attendant, and less than 1% gave birth with a health extension worker. Of note, only 7% of women received postnatal care within 48 hours of birth (6% from a skilled provider, <1% from a health extension worker). Substantially fewer mothers and newborns living in rural areas received postnatal care, compared to those living in urban areas (3% versus 32%) [19].
Low use of postnatal care services by rural Ethiopian women may be due to the tradition of a 40-day period of confinement to protect the mother and newborn from malevolent spirits [16]. However, other community-based projects in Ethiopia and elsewhere have achieved mixed results in terms of improving postnatal care coverage; none have achieved postnatal care coverage greater than 32% [19], even though the utilization of maternal health care service varies with the socio-economic characteristics of the population [20].
Significance of this study is taking in to consideration, that, post-natal health service utilization operates at various individual, house hold and community levels; authors aimed not only evaluating how postnatal care was conducted, but also tried describing why women did not receive postnatal care. Little is known in the study area on current magnitude of utilization of maternity services in health facilities especially postnatal care and associated factors for their utilization to the knowledge of the authors. This study, therefore, tried to assess extent of postnatal care utilization and attempted to describe factors that are assumed to be barriers to postnatal care utilization among mothers who gave birth. It provided relevant information to PNC programmers, Implementers and beneficent.
Objectives
General objective
To assess post-natal care service utilization and associated factors in Asella town, Arsi Zone, Oromiya Regional State, Ethiopia, 2017.
Specific objectives
To determine the prevalence of PNC utilization
To describe the women who utilized PNC in socio-demographic characteristics.
Methods and Materials
Study area and period
The study was conducted in Asella town. Asella is administrative town found in central Ethiopia, west of mount Chilalao. It is located in the Arsi zone which is one of the zones in Oromia Region divided into 26 districts, including two especial Administrative towns, namely Asella and Bokoji. Asella is the capital town of Arsi zone. It is located 175 KM from Addis Ababa, capital city of Ethiopia has a latitude and longitude of 7° 57′N39°7′Ewith an elevation of 2,430 meters. According to Ethiopian national census (CSA 2007), Assela town has a total population of 74,268 of whom 37,337 were male and 36,931 were females [21,22]. The study period was from March 14- September 30, 2017.
Study design
Community based descriptive cross sectional study was conduct to assess PNC utilization.
Population
Source population: The source of population was all households’ mothers in Asella town who gave birth in the last two years whose age is 15-49 years.
Study population: Study of population was systematically select households whose mothers age is15-49 and who gave birth in the last 2 years.
Inclusion criteria: All mothers who gave birth in the last two years and who are volunteer for study
Exclusion criteria: Mothers mentally ill or critically ill, and mothers who lost their children.
Sample size calculation
The required sample size was determined by using simple population proportion formula by considering 33.5% post-natal care service utilization [23].
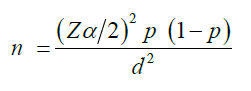
Where,
n= the desired sample size
Zα/ 2 =standard normal score (95%)
p=prevalence of post-natal care service (33.5%)
d=degree of precision desired (5%)
Where,
Z=1.96
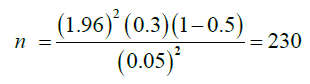
• But since the source of the study subject considered below 10,000 we use the correction formula.
Therefore,
Sampling technique
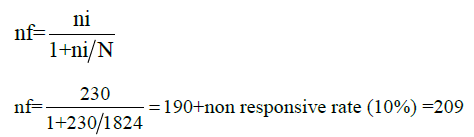
Asella town has fourteen kebeles, among these kebele 09 was select by using Convenience method. There was 1824 total population. Number of females aged 15-49 years is 800.There are seven ketenas in Assela kebele 09. The first ketene was select by using lottery method. Simple random sampling technique was conduct to select couples in each ketenas proportional to their number of currently married couples. The first household was select by lottery method and then K value will be used. K= total households / sample size =800/209=3.8=4 every 4th house hold was interview starting from the end of each village house until the allocated sample achieved. Couples who fulfilled the criteria of the study subject was interview and in the absence of illegible couples in that household the nearby household was interview (Figure 1).
Study variable
Independent variable: Socio-demographic, reproductive factors, knowledge, accessibility
Dependent variable: Utilization of post-natal care
Data collection procedures
Data collection instrument: Data was collected using interview administered structured questionnaire. The principal investigator was involved in the data collection. A structured interviewer administered questionnaire was adapted by investigators after review of different literatures to collect the information based on study objective.
First the questionnaire was prepared in English language and then it was translated to local language (Amharic) and which was again back translated to English. Comparisons were made on the consistency of two versions. The variable to being collected includes socio demographic, economic and question on prevalence of PNC and awareness of people on risk associated with not use PNC.
Data processing and analysis: The Data were entered using EPI-INFO version 3.5.4 and exported to SPSS version 21 for analysis. After it was edited, sorted, organized, and checked for completeness. Descriptive statistics were carried out to characterize the study population using different variables. The result was presented by using table, graph and texts as based on type of data.
Data quality assurance: To assure the quality of collected data the following measure was under taken. The appropriately designed data collection instrument was used. Every day the collected data was cross checked by group members and comments and measures was being undertaken throughout the data collection period for completeness and consistency of the response.
Operational definitions
i. Post-natal care: refers to the assistance given to the mother and the baby for a period of six weeks from the time of delivery.
ii. Utilization of service: It refers to use of post-natal service such as family planning, immunization and other services by women till six months after the delivery of the babies.
iii. Post-natal service: Is the service that consists of immunization, family planning and heath care education on child care, breast feeding, physiotherapy, physical examination, treatment and counseling service.
iv. Immunization: Is the process of administering vaccination to neonates, infant and child.
v. Conceptual frame work; A schematic presentation showing the association between factors and outcomes
vi. Puerperal sepsis: Is infection that occurs after delivery up to six weeks.
vii. Family planning: Is service important for spacing number of pregnancy and prevents unwanted pregnancy.
viii. Traditional birth attendants: Are unprofessional birth attendant who get skill from professionals.
Ethical consideration
Ethical clearance was taken from community and research committee. We were taken permission letter from Arsi University. Permission was being obtained from both the administrator to obtain the desired cooperation and participation.
Verbal informed consent was obtained from each study subject prior to the interview after the purpose of the study is explained to respondent. Confidentiality of the information was being assured and privacy of the respondent was being maintained. The respondents told to have the right to dropout the interview at any time she wishes. At the end of the interview, Information about advantage of postnatal care by skilled health professional explained to the respondents.
Plan for dissemination of finding
The final report will be presented to Arsi University, School of Health science, Department of public health. The result of the study will be disseminated to Assela health desk, Arsi zone health desk through seminar or written formal report. It will also be communicated to Arsi University College of Health Science staff members and students through the university library
Results
Socio demographic characteristics of the participants
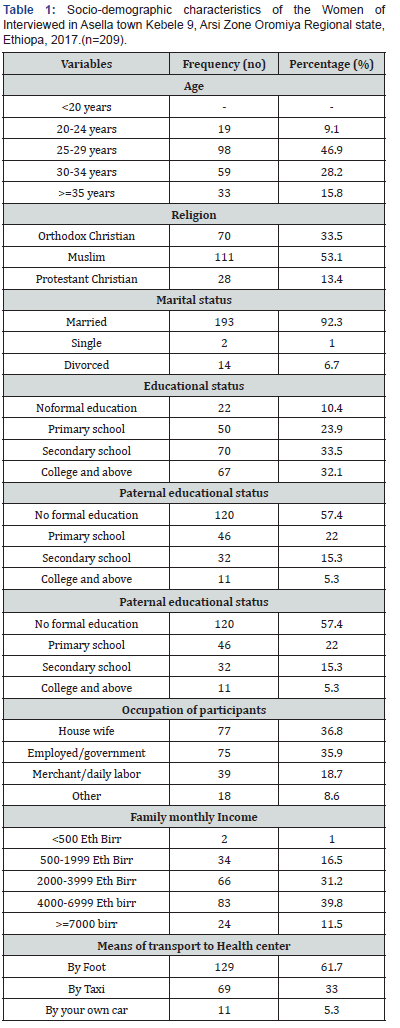
A total of 209 women participated in the study with a response rate of 99.3%. Almost much of (46.9%) of the participants were found between the age of 25 to 29 years. The mean age of the Participants was 26.7 years (+SD=4.4). 111 (53.1%) of them were Muslim and 193 (92.3%) of them were married. With respect to level of education only 67(32.1%) of the respondents had college and above education. The average monthly house hold income was 3948 ETB. More than half 129(61.7%) of the participants were using foot for manse of transportation to the health facilities (Table 1).
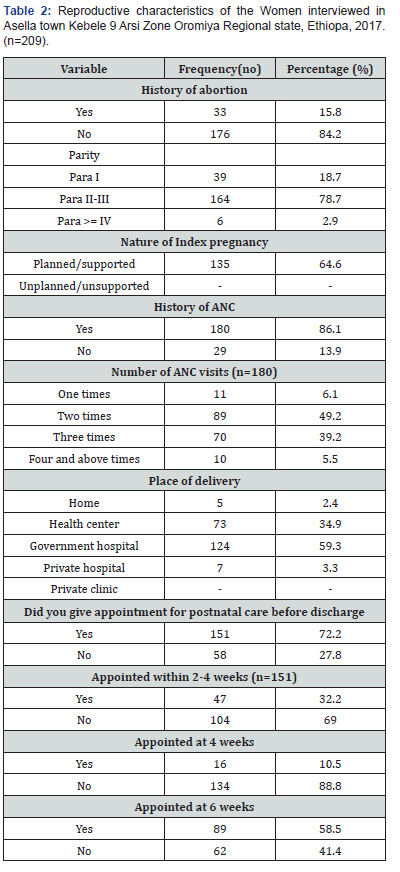
About 176 (84.2%) of the participants didn’t have history of abortion,33(15.8%) have history of abortion. More than Half 164(78.5%) of the participants were multi gravid 135 (64.6%) of the previous pregnancy were Planned and support, 74(35.4%) was unplanned and support. More than half 180(86.1%) respondents had ANC follow up at least one, on top participants were 209(100%). Three fourth 151(72.2%) of the participants were given appointment for postnatal care by the health care professionals before discharge. The remaining 58(27.8%) participants were not informed to have postnatal care by the health professionals before discharge from the health institution. Among women who gave birth 124(59.3%) in governmental hospital, health center 73(34.9%,7(3.3% in privet clinic and home delivery 5(2.4%) (Table 2).
Prevalence of postnatal care utilization
About 152(72.7%) had PNC and 57(27.3%) didn’t have any PNC visit. The most frequent place of postnatal care were at government hospitals 75(49.3%) followed by the health centers 70(46.0%). The proportion of postnatal care visit across 2 weeks of discharge, after four week of discharge and at six weeks of postpartum were 23(15.1%), 65(42.7%) and 58(38.2%) respectively. Contraceptive use after delivery 118(56.4%) Contraceptive initiation period At 6 month 86(71.1%) (Table 3).

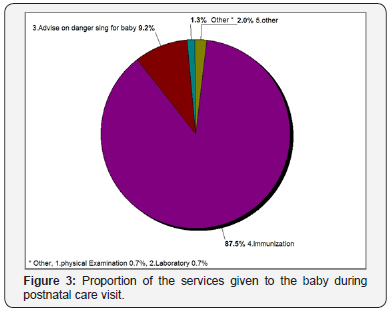
Concerning what was done for the women during postnatal care visit we found that nearly half 56.1% of the respondents provided contraceptives, 3.9% had physical examination,16.8% advice on danger signs, 18.1% provided TT vaccination, and 3.2%had laboratory investigations (Figure 2). Concerning what was done for the baby as it displayed on Figure 3, 87.5% of the babies had received immunization, 9.2% of women were counseled about danger signs of their baby, and only 0.7% of the babies had physical examination and 0.7% laboratory investigation (Figure 3).

Knowledge and awareness about PNC
About 156(74.2%) heard about PNC,53(25.4%) didn’t heard about PNC. From this who heard about PNC from Health works 118(75.6%), 26(16.7%) from mass media,12(7.7%) from neighbor.135(84.1%) know what is given in PNC,21(15.9%) didn’t know.

As shown in the Figure 4 women participated in study know PNC service as immunization 79.7%, Family planning 12.8% and treatment 7.4%.
Determinant of postnatal care utilization
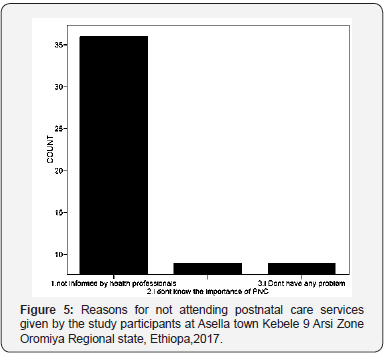
Out of twenty independent variables categorized under Socio demographic, reproductive characteristic, knowledge, Six variables namely educational status, ANC follow up, whether or not PNC appointment given, were determinant of post-natal care utilization in our study (Figure 5). Over all 57(27.3%) of respondents were not using PNC, the major reasons explained by these Women were being not appointed by the health care provider 68.4 % and lack of knowledge on the importance of PNC service and 31.4% (Figure 5).
Discussion
Post-natal care is one of the components of maternal and child health which plays an important role in the prevention of complications that occurs following delivery of the new baby. This study tried to assess the prevalence and knowledge of postnatal care utilization among selected village Assela Town of Arsi Zone, Ethiopia. The selected socio-demographic status of the participants showed most of them 193(92.3%) married, 164(78.5 %) were multiparous and 22(10.4%) were illiterate. This study indicated that (72.7%) of the participants had received a health checkup after delivery despite the fact that almost all women were given birth at health institution 204(97.6%). But this figure is very high when compared with the 2016 EDHS postnatal care utilization rate of 9.0% and 18.8% of institutional delivery rate respectively [5]. This difference might be due to the time difference and the presence of diverse intervention to improvement in accessing and utilizing maternal health care service in the urban area as the case in current study. This study finding on PNC prevalence was also higher than three similar studies conducted in Enderta District, Tigray, 49.7%) [24], Jabitena District, Amhara Region (20.2%) [25], and South Nation and Nationality Region (37.2%) in Ethiopia [26]. The discrepancies might be associated with the variation in the study areas and as well study population.
Similarly, the postnatal care utilization of this study finding also a bit higher when compared to the studies conducted in African and Asian countries; the prevalence of not using postnatal care in Bangladesh (73%), Nepal (72%), Rwanda (71%), Burkina Faso (44%), Cambodia (46%), Haiti (55%), and Kenya (46%) Malawi (41%).
Concerning the quality of postnatal care provided by the health professional, it was found that about more than half (56.1%) of the women were reportedly provided only contraceptives and less than one in three women received the remaining postnatal care services such as counseling on danger signs, physical examination, and health promotion. Similarly, the postnatal care provided to their babies mainly focused on providing immunization (87.5%). The remaining services accounted for less than 11.3 %. This was also true in a study done in southern Ethiopia [26].
The key determinant factor for PNC utilization in our study were educational status, ANC follow up, provision of PNC appointment given by health provider. Women who were counseled and given appointment for postnatal care service were utilized the PNC service higher than those women who didn’t informed about the PNC service on discharge. This was also supported by the reason given by those women who didn’t utilized PNC during this study. Similarly, a study done in northern Ethiopia found that those women who had got information about postnatal care services from Health Extension Workers and Midwife/Nurse had larger oddis (24.87) to attend postnatal care service compared to those women who had got information from other sources [25]. This finding may lead to a conclusion that the PNC service utilization is strongly influenced by the knowledge of women on postnatal care benefits.
Those mothers with secondary levels of education had more postnatal care utilization than mothers who didn’t have formal education. A study done on the assessment of factors affecting utilization of postnatal care services was conducted in Jabitena district, Amhara regional state in Ethiopia found that among the socio-demographic factors, the key predictor for PNC utilization was educational status of the respondents. A participant whose level of education was secondary school and above showed better utilization of PNC service as compared to illiterate women [25,26], similarly a study done in Nepal found that mothers who were educated had better score of using [27].
History of ANC follow up was one of the strongest predictors of postnatal care service utilization mothers who have history of ANC follow up utilize PNC more than women who didn’t have ANC follow up. Another community based study done in northern Ethiopia found that women who had ANC follow up were 4 times more likely to attend postnatal care services as compared to women who didn’t had [28]. A study done in Nepal a woman who had attended a four or more antenatal were more likely to report attending at least one postnatal care visit [27]. This is because it improves the knowledge of better outcome of having post-natal care service.
Strength and Limitation
Strength of the study
The source of the data for this study was based on the selfreport of respondents and provided no validation of obtained information with any objective source such as health facility cards. A high response rate of 99.3% gained from the participants of the study.
Limitation of the study
Using non probability sampling method was one limitation. Recall bias was more likely since women were asked for events which have already happened within the past two years prior to this study despite the consideration of recent births. Study design was descriptive cross sectional and not association done to show determinants. Use of health professionals as data collectors may create bias as they might direct the respondents during the data collection.
Conclusion
The overall prevalence of PNC service utilization in this study was relatively good as compared to Oromiya region 77% of women use post-natal care. In Arsi zone 78% of women use post-natal care utilization in 2009, also the same in Tiyo woreda, but it is very high compare to EDHS 2016 Oromyia 9.0% of women had postnatal care in the first 2 days after delivery. To enhance PNC service utilization all women should be counseled about postnatal period and provided appointment. The health care providers and policy makers are recommended to increase the awareness mothers on postnatal care services, to prevent maternal and neonatal complication and to schedule mothers based on the national postnatal care follow-up protocol in order to increase post-natal care service utilization.
Recommendations
a. To health professionals: Should be counsel about the danger signs of postnatal period and give appointment for PNC.
b. To health facilities: Should assure comprehensive and quality of postnatal care services. Should give continuous training for health care providers on PNC appointment and counseling about danger sign during postnatal period
c. To Health bureau: Should emphasize the improvement of quality of service PNC utilization. Should prepare guide lines on danger sign during Post-natal care visit.

Comments
Post a Comment