Ultrasound Diagnosis of Exomphalos (Omphalocele): Differentiating Exomphalos from Normal Physiologic Gut Herniation and Gastroschisis-juniper publihers
Authored by: Jitendra Parmar*
Introduction
An Exomphalos, also known as omphalocele is a congenital midline abdominal wall defect at the base of umbilical cord insertion with herniation of gut and/or liver or occasionally other contents, out of the fetal abdomen. Many chromosomal anomalies are often associated with this embryologic defect [1-6]. A gastroschisis is a ventral abdominal wall defect, almost always to the right of the umbilicus from which it is separated by thin skin bridge, and contains abdominal viscera, most commonly small bowels, stomach and gonads without coverings [7,8]. During first trimester sonogram, normal physiologic herniation of the fetal bowel seen oftenly between 8 and 12 weeks gestational [9]. With careful detail scanning, the sonographer may be able to differentiate normal physiologic gut herniation from early identification of exomphalos and gastroschisis [9,10]. This case report describes a ultrasound diagnosis of exomphalos associated with hypoplastic nasal bone and increased nuchal translucency and discusses how to differentiate exomphalos from normal physiologic gut herniation and gastroschisis.
Case Report
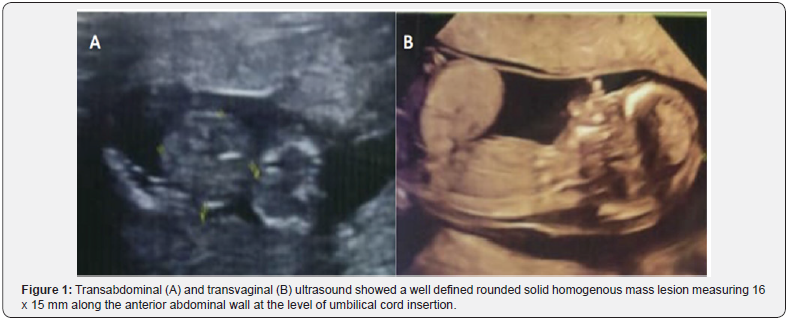
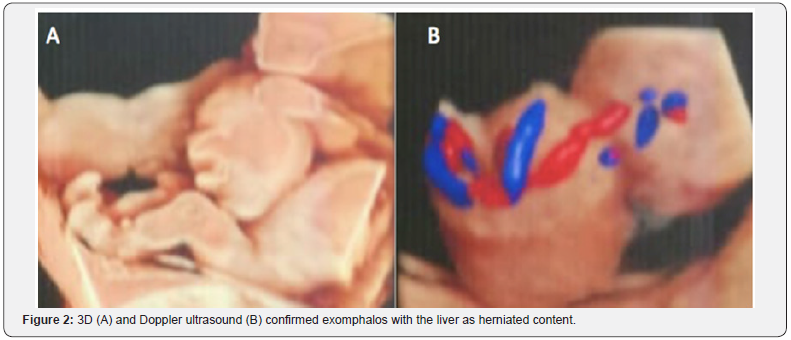
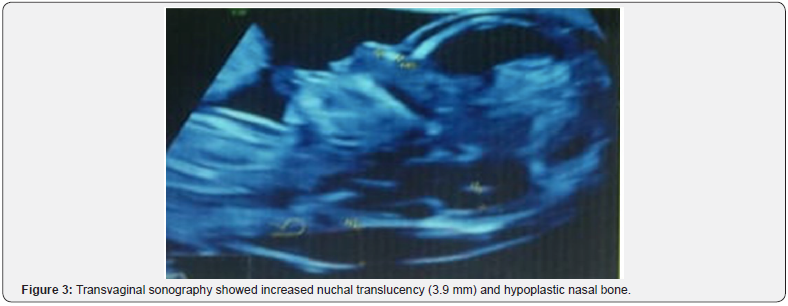
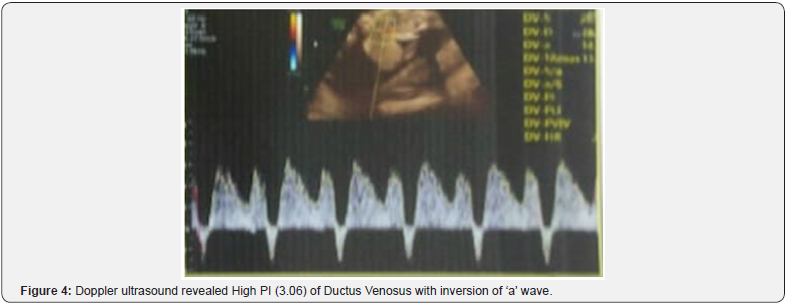
A 27-year-old woman having her first pregnancy, at the 12 weeks + 4 days was referred to the ultrasound (US) department for a routine US without any pertinent past medical history. Transabdominal US, followed by transvaginal US was performed using a 2D (two dimensional) and 3D (three dimensional) ultrasound equipment (Voluson E 10 BT 17; Probe 3.5 MhZ). 2D US showed a single live intrauterine pregnancy with gestational age of 12 weeks + 4 days. A well defined rounded solid homogenous mass lesion, measuring ~ 16 x 15 mm seen at the umbilical cord insertion site (Figure 1). By using Doppler US and 3D US, an exomphalos containing the liver was identified (Figure 2). US also showed increased nuchal translucency, 3.9 mm and a hypoplastic nasal bone (Figure 3). Ductus Venosus shows increased PI (3.06) with reversal of ‘a’ wave (Figure 4). Detailed US for possible associated malformations could not find any other structural defects. The detail ultrasound parameters are described in Table 1. As a result of the sonographic findings the patient terminated the pregnancy, and no follow-up was able to be obtained. It is unknown whether the patient had the products of conception tested for aneuploidy.
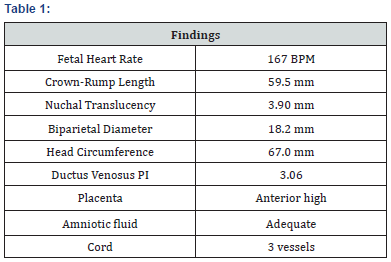
BPM: Beats Per Minute
Mm: Millimetre
PI: Pulsatility Index
Discussion
An exomphalos is an encapsulated ventral wall defect containing liver and/or bowel and occurs because of incomplete rotation of bowel returning into the abdominal cavity. The translucent sac, which is composed of the Wharton jelly, amnion and the peritoneum, contains the abdominal viscera with well visualization of the radiation of the umbilical vessels onto the sac wall. In ~ 50% of the cases, the herniated bowel accompanied with the liver, spleen, ovaries or the testes [7,8]. According to contents of herniation, exomphalos may be categorized as those containing both liver and bowel (extracorporeal liver) and those containing only bowel (intracorporeal liver). Intracorporeal exomphalos can only be reliably diagnosed after 12 weeks, because of the difficulty in distinguishing it from physiologic midgut herniation [11,12]; Such exomphalos have a high rate of foetal chomosomal abnormalities [13,14]. Extracorporeal exomphalos can be diagnosed as early as 9 to 10 weeks, and these may also be associated with fetal chromosomal abnormalities and other birth defects [15-17].
Exomphalos frequently have been associated with other conditions, such as congenital heart disease, cleft palate, musculoskeletal abnormalities, intrauterine growth restriction and dental malocclusion. The incidence of associated chromosomal abnormalities is 10-40% that include trisomies 12, 13, 15, 18, and 21.3 [18-22]. A featus found to have an exomphalos has a high mortality rate because of its coexistance with multiple anomalies [9,23]. However, because of improvement in the parenteral nutritional, surgical and the anesthetic management techniques, the survival of the exomphalos cases has increased from 60% during the 1960s to more than 90% at present [7,24].
The diagnosis of exomphalos can be made by ultrasound in 1st trimester; however, two close differentials; gastroschisis and physiologic midgut herniation, need to be excluded by careful and detail imaging. One of the most important and specific finding to differentiate exomphalos from midgut herniation is the visualization of herniated liver associated with gut loop within the herniated sac. Few other significant secondary features that differentiate physiologic midgut herniation from exomphalos: by 12 weeks gestational age, midgut herniation descends back into the abdominal cavity; exomphalos have homogenous appearance, while midgut herniation tends to have heterogenous appearance; exomphalos presents as a large circular shaped lesion measuring more than 7 mm, while midgut herniation presents as a small spherical shaped lesion measuring ~ 4 to 7 mm. Gastroschisis occurs later because the anterior abdominal wall defect before 16th week is very small and anterior abdominal wall muscles and peristaltic waves are visible only in 14th week. Intestinal convolutions pass through a small defect (<1 cm), which is localized to the right of the normal umbilical cord insertion and float freely in the amniotic fluid with no membrane covering the content [25].
In cases with difficulty to identify the exact pathology and to demonstrate the co-existing pathologies, the 3D USG may be helpful. Besides its help as a diagnostic tool, the 3D ultrasound may help the family to understand and realize the situation. The decision process, genetic counselling, perception of the situation and its importance, future planning and the state of the management will be affected by the thorough comprehension and concern of the family. First trimester scanning of the anterior abdominal wall is crucial and at most important. It is important to determine the gestational age of the featus being examined. The sinologist must examine the echogenicity of the herniation at the base of the umbilicus and make a determination as to heterogeneity or homogeneity and whether covering present or absent. Measurements must be taken at the base of the umbilical herniation, if the herniation is too large to be considered a physiologic midgut herniation. As the exomphalos is not usually an isolated finding, a survey must be used to further identified other potential abnormalities.


Comments
Post a Comment