Meconium Peritonitis by Segmental Volvulus of the Ileum, Prenatal Diagnosis: Clinical Finding and Literature Review
Global Journal of Reproductive
Medicine Juniper
Publishers
Authored by: Rajaonarison JJC*Abstract
Introduction: Meconium Peritonitis is a chemical inflammation of the peritoneum resulting from in-utero bowel perforation. The aim of this clinical study was to identify the antenatal management and outcomes.
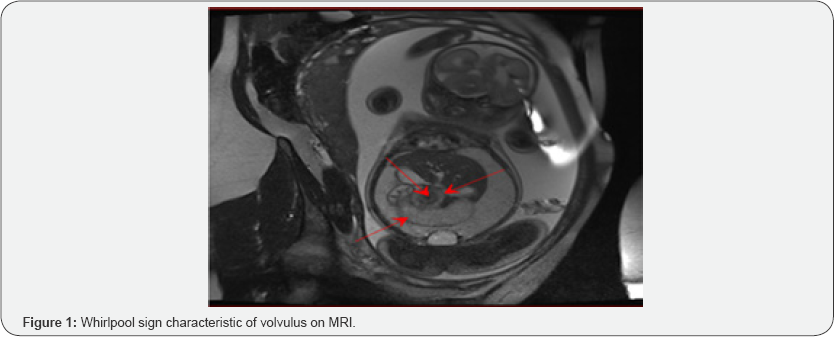
Observation: A case of antenatally diagnosed meconium peritonitis by segmental volvulus of small bowel was reported. A meconium ascites was detected at 22Wks of a second pregnancy on a woman who, to date, had shown neither any complication nor any medical history. The investigation for dyschromosomia, mucoviscidosis, viral infections, cardiac malformation and fetal alloimmunization was negative. The ultrasound and MRI conducted at 30Wks and 1 day of gestation had confirmed the volvulus perforation of the small bowel terminal loop with an appearance of « Whirlpool sign », and probably associated with digestive ischemia. A cesarean section was planned at 37Wks and a surgical diagnosis had confirmed the volvulus.
Discussion and conclusion: MRI scan could serve for a prenatal diagnosis of a volvulus with a « Whirlpool » sign. Severe associated pathologies should also be investigated.
Keywords: Prenatal Diagnosis; Meconium peritonitis; Ileal volvulus
Introduction
Meconium peritonitis is a medical condition of the inflammatory chemical peritonitis resulting from in utero bowel perforation [1]. All pathologies leading to intestinal obstruction or a necrosis of the intestine wall and viral infections may be incriminated [2]. The mortality rate associated to this disease ranges from 2,4 to 50% and the morbidity around 34% [3]. The aim of this study was to report a case of antenatally diagnosed meconium peritonitis by segmental volvulus of ileum in order to manage the neonatal outcomes.
Observation
A meconium ascites was identified through a morphology scanning conducted at 2 2 Weeks of amenorrhea (Wks.) in a 28-years-old G2P1 patient with no previous specific medical history. Prenatal genetic testing revealed a normal karyotype (46XY) and no chromosomal abnormalities. Investigation of specific mutation gene of mucoviscidosis was negative. Serum screenings for viral infection were also negative for hepatitis, rubella, CMV, PV B19. An ultrasound had been performed at 30 Wks of gestation when the patient was admitted to the Centre. It revealed an ileal dilation of 12mm with a reduced intestinal transit, residual meconium ascites tends to form polyhydramnios beyond the normal level. MRI performed on the same day had confirmed the presence of a segmental volvulus on the small bowel terminal loop with a «Whirlpool sign » feature and probably associated with a digestive ischemia, excluding the incidence of any related malformation (Figure 1). Ultrasound examination conducted at 33Wks and 4 days of gestation revealed a voluminous stomach, and dilated intestinal loops of 20mm containing meconium fluid. Intestinal transit and Doppler indices were preserved. Furthermore, there were a hyperechogenic mass in the right iliac fossa, with tubular structures but with no peristalsis that could indicate an ischemic necrosis on parts of the loops, and organized meconium ascites (Figure 2).


The meconium ascites always remained in a stabilized form and a polyhydramnios with a Chamberlain's line of 9cm was noted. Ultrasound imaging performed at 36Wks and 3days of gestation had shown a regression of the ascites and a stability of the fetal digestive lesion while the MRI enabled to confirm normal cerebral gyri. The neonate was extracted by cesarean section at 37Wks and 1day of gestation to facilitate neonatal cares. A male infant was delivered with an Apgar score of 10 at the first, the fifth, and tenth minutes, weighing 2975g, pH 7,26, lactates 2,11. That infant showed a good adaptation to the ex utero life. Mild abdominal distension was noticed. An planned abdominal X-ray revealed images of intraperitoneal calcifications, dilation of digestive tracts, and obstruction at the proximal loop of the ileum. An exploratory laparotomy set at 36h after birth confirmed the necrosed loop of the ileal volvulus which is reduced to a banded knot, a digestive dilation of the upper section extending to 60 cm from the ligament of Treitz and an atresia at the lower section up to 25cm of the healthy bowel, attaining the ileoceacal valve and the entire colon (Figure 3). The necrosed loop was resected, it had a length of about 30cm. An ileostomy of the right flank was performed because of the variability of gut size, the residual ileum measures 85cm. To close up the stoma, a termino- terminal anastomosis was performed at 45 days after birth with a favourable result. The growth curve is normal after a delay of 18 months.
Discussion
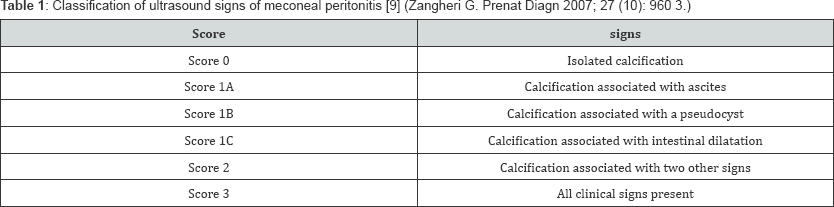
The reported case from this observation strengthen effectiveness of prenatal diagnosis, significance of multidisciplinary consultation in a maternity ward of university hospital and illustrate pediatric management of meconium peritonitis by segmental volvulus of the small bowel. Antenatal volvulus is a rare occurrence [4]. Intestinal atresia, a tight mesentery, or an intestinal malrotation are common cause of volvulus as it may be primitive [5]. It may also arise from digestive duplication, mesenteric defect, an abnormality of the intestinal muscles or a cystic fibrosis [6]. Early sign of meconium peritonitis is revealed by the as cites imaging. It occurs in all cases [7]. Images related ton intestinal hyperechogenicity or calcium deposition inside peritoneum may be faulty on the onset of the disease but when it appears, it is characteristic. Calcifications resulted either from the deposit of calcium or from the inflammatory reaction of keratins with meconium [2]. Other ultrasound findings include, intestinal dilatation (57%), pseudocyst imaging (29%), polyhydramnios (50%) [7], fetal hydrops (10%) which, as being reported, was linked with a Parvovirus B19 infection [8], or also to a meconium hydrocele [6]. Zangheri G had described a scoring system to categorize prenatal ultrasound findings of meconium peritonitis [9] (Table 1).
While diagnosis of meconium peritonitis seems to be simple and well known, that of ileum segmental volvulus is difficult. Diagnosis is conducted randomly during prenatal period. Most of the time, findings are nonspecific. The pathognomonic sign of a volvulus is the whirlpool configuration which was already described by many authors [10]. Such sign was discovered on the fetus of our patient. At birth, the obstruction was evidenced by an abdominal distension which is worsened with a respiratory distress or even a hypovolemia. It may evolve to bilious vomiting. Lack of meconium emission is nonspecific. A plain X-ray of the abdomen showed a dilation of the loops, images of calcifications inside the abdomen and hydroaeric imagings related to small bowel occlusion. Meconium may also make its way to the vagina by attaining the fallopian tube or out of the Douglas's pouch perforation [11].
When a meconium peritonitis is suspected by ultrasound, the aetiology is immediately established. Screenings for viral infections are examined particularly those of Cytomegalovirus,Parvovirus B19 which may be associated with liver calcifications, rubella, chickenpox, and viral hepatitis [12]. The determination of mucoviscidosis by investigating any specific gene mutation is mandatory as it appears in 7,7 to 40% cases of meconium peritonitis [1]. The karyotyping and a genetic study of the chromosomes are indicated. The diagnosis of any malformation is conducted systematically using fetal MRI scan. Besides, it is more accurate than the ultrasound finding when it regards to diagnose meconium peritonitis (57,1 vs 42%) [13]. Other indices of fetal as cites as cardiac malformation, or alloimmunization are as well performed systematically. A paracentesis study of histology and biochemistry of the fetal as cites fluid is also indicated [14].
These investigations support the prenatal monitoring, obstetrical decision-making, predicting and neonatal management of patients. Termination of pregnancy could eventually be considered in case of mucoviscidosis or any chromosomal abnormality. Monitoring must be conducted by achieving puncture aspiration which may be useful to circumvent a pulmonary hypoplasia. If polyhydramnios is not tolerated by the fetus, a puncture aspiration could be suggested as it reduces the risk of premature delivery. Induction of prematurity is only established when the fetus manifests a clear sign of anoxia or a case of aggravated as cites and intestinal dilation arise, requiring an emergency neonatal surgery [12]. Benefit of cesarean section on the neonatal prognosis is not documented. Monitoring must be closely followed up by obstetrical ultrasound. Any complication sign as as cites and polyhydramnios is diagnosed by ultrasound, the growth of the fetus, and its tolerance of the as cites is appreciated by recording fetal heart rate. In case of abundant as cites formation, some authors perform a puncture aspiration of the fluid during labor to avoid occurrence of abdominal dystocia and to allow a normal vaginal delivery [1].

Comments
Post a Comment