Clinical Dilemmas and Risks of Misdiagnosis and Mismanagement Associated with Endogenous Caesarean Scar Pregnancy: A Case Series and Literature Review
Global Journal of Reproductive Medicine Juniper Publishers
Abstract
A caesarean scar pregnancy (CSP) is a pregnancy that
implants into the myometrium at the site of a previous uterine incision.
In this paper, we present three cases of women affected by caesarean
scar implantations. Each case presented differently and was managed in
separate ways. We describe their differing presentations and care as
well as reflecting on how such women may be better cared for. Endogenic
CSPs grow into the uterine cavity and can easily be mistaken for a
normal pregnancy implantation. Differentiation can often only be seen at
early gestations. All women with a previous uterine scar should
potentially be offered early trans-vaginal ultrasound to correctly
diagnose the implantation site. However, in many women, the diagnosis is
not suspected until a complication arises. We advocate for there to be a
higher index of suspicion for CSPs during early pregnancy ultrasound
and that all practitioners performing such scans should be trained to
allow a confident diagnosis of CSP.
Keywords: Caesarean scar pregnancy; Caesarean sections; Intravenous; Ultrasound scan; Human chorionic gonadotrophin
Abbreviations:
CSP: Caesarean Scar Pregnancy; TVS: Trans Vaginal Ultrasound; CS:
Caesarean Sections; TOP: Termination of Pregnancy; MVA: Manual Vacuum
Aspiration; IV: Intravenous; A&E: Accident &Emergency; TAS:
Trans Abdominal Scan; UV: Ultrasound Scan; HCG: Human Chorionic
Gonadotrophin
Introduction
Caesarean scar pregnancy is defined as implantation
into the myometrium defect occurring at the site of the previous uterine
incision. The prevalence of CSP is estimated to be approximately 1 in
2000 pregnancies and these pregnancies may be ongoing potentially viable
pregnancies or miscarriages within the scar. 37 The diagnostic criteria
described for diagnosing caesarean scar implantation on transvaginal
ultrasound include:
I. Empty uterine cavity.
II. Gestational sac or solid mass of trophoblast
located interiorly at the level of the internal as embeded at the site
of the previous lower uterine segment caesarean section scar.
III. Thin or absent layer of myometrium between the gestational sac and the bladder
IV. Evidence of prominent trophoblastic/placental circulation on Doppler examination.
V. Empty endocervical canal.
Thirteen percent of reported ca SES of CSP were
misdiagnosed as intrauterine or cervical pregnancies at presentation.
The true prevalence of caesarean scar pregnancies is likely to be
somewhat higher than estimated in the literature as some cases will end
in the first trimester, either by miscarriage or termination, and go
unreported and undiagnosed. There is a spectrum of severity CSP is
defined as implantation into the myometrial defect occurring at the site
of the previous uterine incision. The prevalence of CSP is estimated to
be approximately 1 in 2000 pregnancies and these pregnancies may be
ongoing potentially viable pregnancies or miscarriages within the scar.
The diagnostic criteria described for diagnosing caesarean scar
implantation on transvaginal ultrasound include:
i. Empty uterine cavity.
ii. Gestational sac or solid mass of trophoblast
located anteriorly at the level of the internal os embedded at the site
of the previous lower uterine segment caesarean section scar.
iii. Thin or abse nt layer of myometrium between the gestational sac and the bladder.
iv. Evidence of prominent trophoblastic/placental circulation on Doppler examination.
v. Empty endocervical canal.
Thirteen percent of reported cases of CSP were
misdiagnosed as intrauterine or cervical pregnancies at presentation.
The true prevalence of caesarean scar pregnancies is likely to be
somewhat higher than estimated in the literature as some cases will end
in the first trimester, either by miscarriage or termination, and go
unreported and undiagnosed. There is a spectrum of severity. A caesarean
scar pregnancy (CSP) is a pregnancy that implants into the myometrium
at the site of a previous uterine incision. They are one of the rarest
forms of ectopic pregnancy with an incidence of 1:1800 pregnancies [1].
Such pregnancies may result either in an early miscarriage or a viable
ongoing pregnancy within the scar. Since the first report by Larsen and
Solomon in 1978 [2], the incidence of these pregnancies has been increasing, reflecting rising caesarean section rates.
The natural history of such pregnancies has not been
fully elucidated. The morbidity and early indicators of outcomes are yet
to be fully described. It is suggested placenta acreta is the end point
of an ongoing caesarean scar ectopic pregnancy [3]. Management options are variable and the best way to prevent recurrence unclear [4].
As with other non-tubal pregnancies misdiagnosis is common resulting in
mismanagement and poorer outcomes. In addition to a comprehensive
history, transvaginal ultrasound (TVS) is the primary modality for
diagnosis. A recent RCOG guideline has emphasized ultrasound diagnostic
criteria, however, these have not been validated [4].
In this paper, we present three cases of women affected by caesarean
scar implantations, describing their presentation and management as well
as reflecting on how such women may be better cared for.
Case Study 1
A 30-year-old Afro-Caribbean, gave a history of two
previous caesarean sections (CS) and a first trimester termination of
pregnancy (TOP). The surgeon performing her last CS had advised her
against future pregnancies due to a very thin lower segment. As a
result, when she inadvertently fell pregnant she opted to terminate the
pregnancy. TVS at the local TOP service suggested that the pregnancy was
'outside the womb' and referral was made to a neighbouring early
pregnancy unit where she was scanned by a sonographer. TVS here showed a
viable seven-week intrauterine pregnancy with an irregularly shaped
gestational sac. Consequently, she returned to the termination service
for her surgical procedure at 9 weeks and 3 days. She underwent a manual
vacuum aspiration (MVA) under sedation. This was complicated by heavy
vaginal bleeding and the operator was concerned about a possible uterine
perforation. The patient was given uterotonics (syntocinon 5+51U IV,
misoprostol 1mg PR) as well as intravenous (IV) tranexamic acid (1g). A
vaginal pack was inserted and ambulance transfer to our accident and
emergency (A&E) resuscitation room was arranged.
On arrival, her blood pressure was 96/58mmHG with a
heart rate of 89bpm, her haemoglobin estimation was 70g/dL. A
transabdominal ultrasound scan (TAS) showed a bulky uterus with a clot
in the cavity and a second mass, presumed clot, above the fundus. She
was consented and transferred to theatre. She underwent laparoscopy with
Palmers point entry. There were dense adhesions from her previous CS
scar resulting in the uterus being attached to the anterior abdominal
wall. These adhesions were divided and the bladder reflected, revealing a
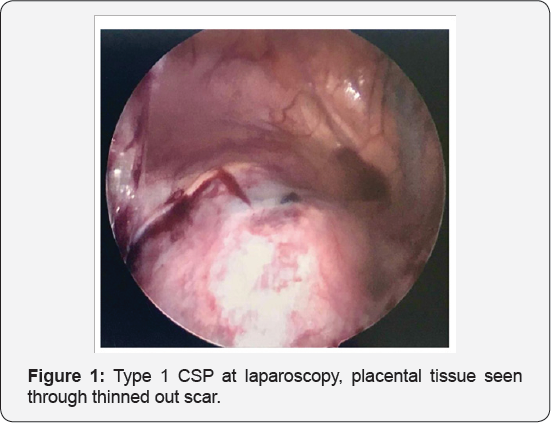
thinned out lower segment scar and a ballooning above the cervix (Figure 1).
A diagnosis of a CSP was made. Using a harmonic scalpela the lower
segment of the uterus was opened and the placental bed site excised. A
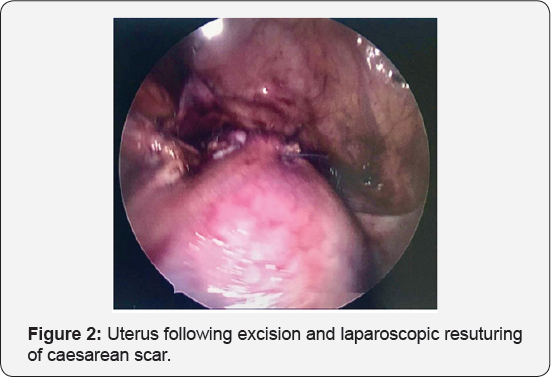
400ml blood clot was removed from inside the uterus and the defect was
closed in 2 layers, with intracorporeal no 1 polysorb suturesa (Figure 2).
She was transfused three units of red blood cells and discharged home
on day five. Human chorionic gonadotrophin (HCG) levels had normalized
by day 40 and she was advised to avoid pregnancy for at least six
months. Histopathological examination of the excised portion confirmed
placental implantation site tissue.
Case Study 2
A 41-year-old woman South Asian lady presented with a
history of two full term deliveries, the first by CS for breech
presentation and the second by spontaneous vaginal delivery. She had had
five miscarriages and one surgical TOP. One of the miscarriages was of a
molar pregnancy. Her initial presentation to our EPAU was with groin
pain. A TVS showed a viable intrauterine pregnancy of 7 weeks and 6 days
gestation and an HCG level of 61,016. The pregnancy sac was noted to be
low just above the cervix. Three weeks later she attended an off-site
clinic requesting surgical TOP for social reasons. She underwent MVA
under sedation. She bled 300ml during the procedure and then collapsed
in recovery with a further bleed of 500ml. She was given uterotonics
(syntocinon 5IU IV and syntometrine 5IU IM) and IV tranexamic acid (1g).
A vaginal pack was inserted and she was transferred via ambulance to
our units A&E resuscitation room. Upon arrival, she had a heart rate
of 91 and blood pressure of 126/59, bedside haemoglobin estimation was
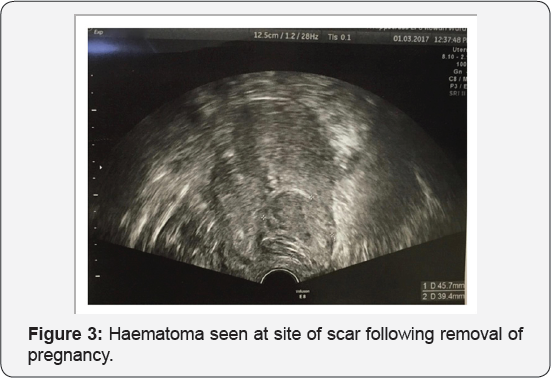
67g/dl. TAS at the bedside showed a haematoma at the site of the
previous caesarean scar but no intra-abdominal free fluid. The vaginal
pack was removed and she was given 1mg of rectal misoprostol and a 40IU
infusion of syntocinon. Bleeding settled and she was transferred to our
ward for observation and transfusion of three units of red blood cells.
HCG was 4225mIU/ml. TVS the following day showed a 45x45x39mm caesarean
scar haematoma (Figure 3), repeat scan 6 weeks later showed complete resolution of this lesion.
Case Study 3
A 38-year-old Caucasian lady, presented with
abdominal pain, vaginal bleeding and a positive urinary pregnancy test.
She gave a history of one previous CS for foetal distress five years
previously. TVS showed a gestational sac implanted low in the uterine
cavity with early foetal demise. Subsequent TVS performed by a
consultant, immediately prior to a scheduled MVA procedure, showed a
very vascular and irregular gestational sac measuring 42x32x45mm lying
low in the uterus near the CS scar with only a thin layer of covering
myometrium. A CSP was suspected and a decision was made to perform an
evacuation of retained products of conception under general anaesthetic
in anticipation of potential complications. A suction evacuation was
performed with ultrasound guidance. The theatre team were prepared for
large blood loss and appropriate blood products had been made available.
Following removal of the pregnancy there was brisk bleeding. TAS
confirmed an empty cavity and there was no suspicion of perforation. She
received misoprostol (1mg PR), syntocinon 5+5iu IV and 40IU infusion,
carboprost IM 250mg twice and IV tranexamic acid (1g) alongside bimanual
compression for 10-15 minutes compression. Her bleeding settled with a
measured blood loss of 2250ml. Starting haemoglobin was 138g/dl, she
received two units of red blood cells and haemoglobin following these
was 113g/dl. She remained on the ward overnight for observation and was
given three, four hourly doses of oral misoprostol. There was no further
blood loss she was discharged the following day.
Discussion
CSPs are a relatively modern phenomenon. The
increasing incidence is thought to be either due to increased reporting
or increasing global caesarean section rates. The symptoms of CSP do not
differ from those of other non-tubal pregnancies but they occur
exclusively in women who have had previous CS, occurring in about 6.1%
of women with an ectopic pregnancy and at least one CS [5].
The pathophysiology of caesarean scar pregnancies remains unclear. It
is likely that a CSP forms following invasion of the implanting
blastocyst through a microscopic niche in the healed uterine scar.
Additionally, there may be a more global impact on the endometrium due
to the very presence of scar tissue which allows aberrant implantation [6].
CSPs form a clinical spectrum from a partial implantation over a thick
scar, which grows into the uterine cavity, to a pregnancy fully located
outside the uterine cavity, only connected to the uterine cavity via a
thin tract. Two main types have been described [7].
The first type, also known as type 1 or endogenic,
implants over the scar but proceeds to develop within the uterine
cavity. It may appear as a viable intrauterine pregnancy, complete with
yolk sac, embryo and cardiac activity, and progress to a viable
gestational age with possible problems with placentation [8].
Type 2 or exogenic scar ectopics are pregnancies that implant more
deeply within the scar and grow in the direction of the serosal surface
of the uterus towards the broad ligament or bladder. A thin layer of
myometrium may be seen at early gestations between the gestational sac
and the serosa. In two thirds of cases this will measure less than 5mm [9].
As the pregnancy grows this layer thins and disappears. Consequently,
the pregnancy bulges through the scar defect with a much greater rate of
early uterine rupture and subsequent haemorrhage
Ultrasound remains the most used modality for diagnosis. A recent guideline from the RCOG [4] describes criteria for diagnosis which include:
a. Empty uterine cavity.
b. Gestational sac or solid mass of trophoblast
located anteriorly at the level of the internal os embedded at the site
of the previous lower uterine segment caesarean section scar.
c. Thin or absent layer of myometrium between the gestational sac and the bladder.
d. Evidence of prominent trophoblastic/placental circulation on Doppler examination.
a. Empty endocervical canal: Ultrasound can also be
used to differentiate between type 1 and type 2 CSP. In endogenic (type
1) CSP, the deformity seen on ultrasound is less apparent as the
implantation grows towards the uterus. The ultrasound image consequently
can appear as a viable intrauterine pregnancy [10].
In these types of low implantation endogenic CSP, differentiation from a
normal pregnancy can often only be made by ultrasound at earlier
gestations [3]. For optimal management of CSP a high index of suspicion and early diagnosis is the key to successful outcomes [11]. This also allows women to make informed choices based on potential morbidity [4].
As a rule of thumb, taking the woman's wishes into consideration, CSP
diagnosed at early gestation should be terminated. The decision is
easier for non-viable or unwanted pregnancies as opposed to wanted
pregnancies where a heartbeat is identified on scan. Though there have
been reports of successful deliveries an expectant approach increases
the risk of a morbidly adherent placenta with likely caesarean
hysterectomy and significant haemorrhage [12-15].
An additional question raised by 2 of our 3 cases is
whether it is safe for women who want to have a TOP and have a history
of CS to have this performed in community based TOP centres or whether
they should be performed in centres with options for laparoscopic
surgery or intensive care facilities should the need arise.
There are very few randomised studies of the management of CSP. Most evidence comes from case series and reviews [4], there is one systematic review of outcomes [16]. Current evidence regarding differing management options has recently been reviewed [6].
Conclusion
Literature suggests that we are not over diagnosing
caesarean scar pregnancies. Most case reports, including our own,
describe situations where the diagnosis was only suspected following
significant maternal bleeding after instrumentation of the uterus for
management of a miscarriage or termination. The key to the diagnosis is a
high index of suspicion and a TVS performed by an appropriately
experienced and skilled operator. Up to 13.6% of CSPs are misdiagnosed
as an inevitable miscarriage or a cervical ectopic [6].
Interventions in such cases without the necessary preparations for
major haemorrhage can lead to increased morbidity and hysterectomy.
Strong Doppler colour flow and the presence of the 'sliding sign'
differentiates a scar ectopic from a low lying inevitable miscarriage.
Ballooning of and a sac within the cervix are the hallmarks of a
cervical ectopic pregnancy.
We recommend that all women with a history of
caesarean section are referred for an early viability TVS with an
appropriately skilled sonographer or gynaecologist to rule out a
diagnosis of caesarean scar ectopic. This should be performed before
routine dating scans, to allow time for counselling and management
should a CSP be diagnosed. To facilitate this; sonographers, nurse
specialists and doctors performing these scans in early pregnancy units
should be encouraged to consider the diagnosis and be appropriately
trained in the ultrasound diagnosis of CSP. We recommend that all women
undergoing TOP with a caesarean section scar site implantation or
suspected Caesarean ectopic pregnancy have their procedure performed in
units with facilities not only to cope with major haemorrhage but also
to perform laparoscopic surgery should this be needed.
Additional Files
To Know More About Please Click on: Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Journals Publishers Please Click on: Juniper Publishers

Comments
Post a Comment